CHAPTER 14 GASTROINTESTINAL PATHOLOGY
ESOPHAGUS
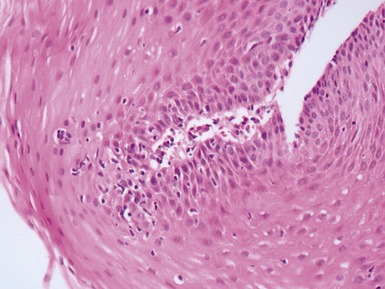
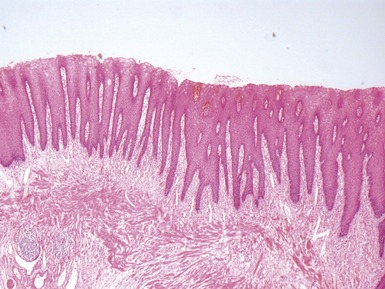
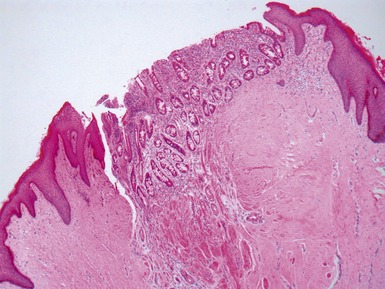
HISTOLOGICAL VARIANTS OF NORMAL ESOPHAGUS
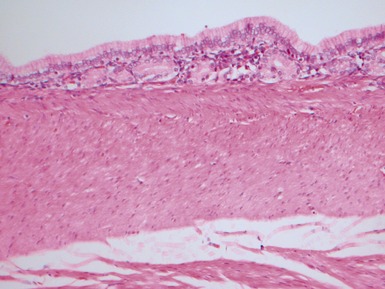
• Normally lined by non-keratinizing squamous epithelium but several normal variants may occur
ESOPHAGEAL ATRESIA AND TRACHEO-ESOPHAGEAL FISTULA
Histopathological features (Dutta, Mathur, Bhatnagar 2000)
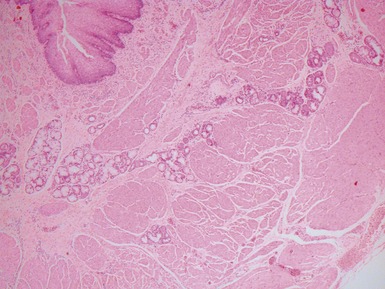
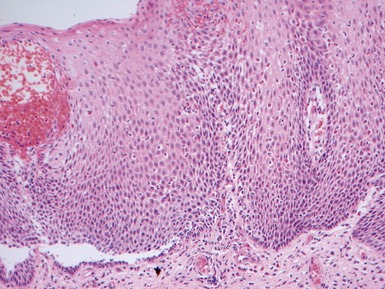
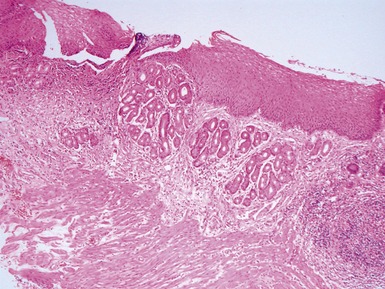
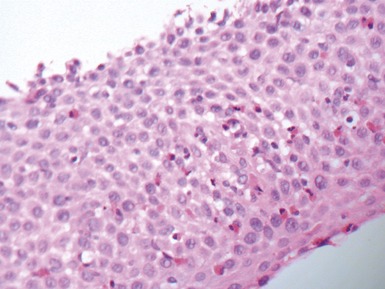
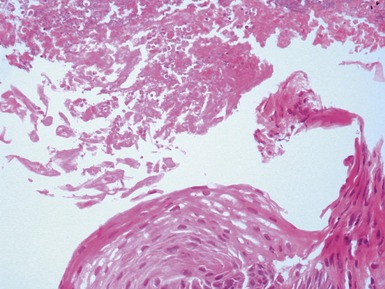
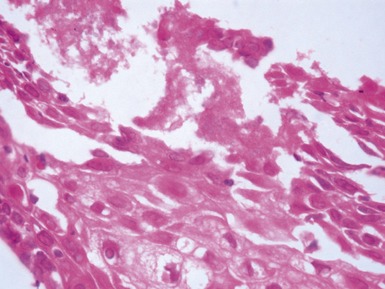
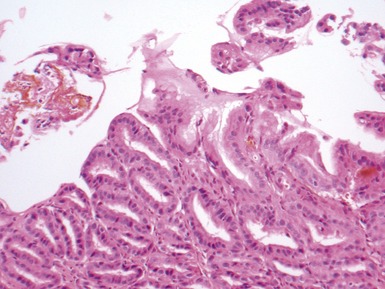
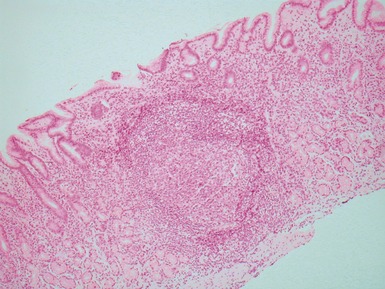
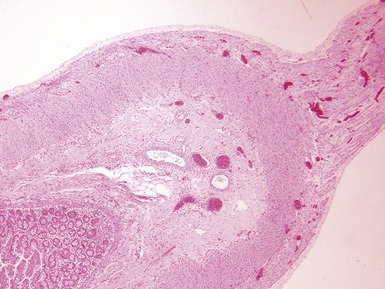
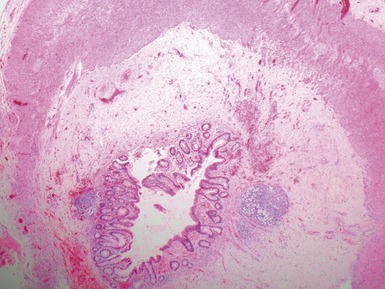
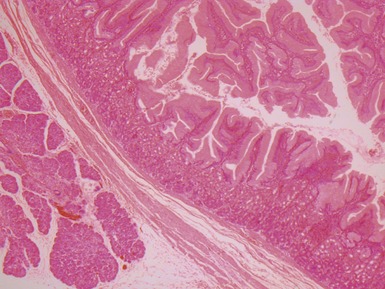
• When submitted tissue comprises elements of tracheal and esophageal wall in variable combinations according to case (Figs 14.2, 14.3)
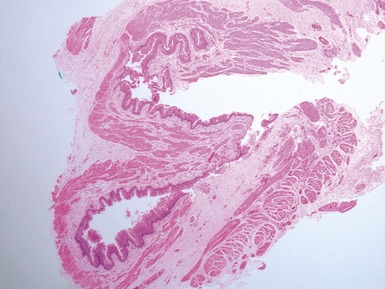
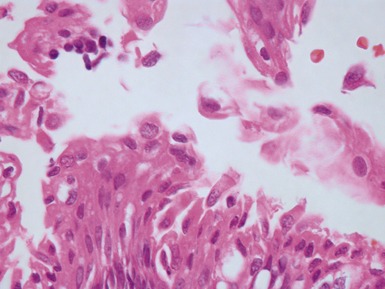
Fig 14.2 One-day-old girl with esophageal atresia and tracheo-esophageal fistula. The specimen is the tip of the proximal esophageal pouch. Photomicrograph of the specimen demonstrating the pouch comprising the usual elements of esophageal wall. The mucosa shows some ciliated epithelium. Unusually, no striated muscle was present in the muscular coat.
GASTRO-ESOPHAGEAL REFLUX DISEASE
• GER of sufficient severity to cause symptoms or disease is termed gastro-esophageal reflux disease (GERD)
COLUMNAR EPITHELIAL LINED ESOPHAGUS (CELE)
INFECTIVE ESOPHAGITIS
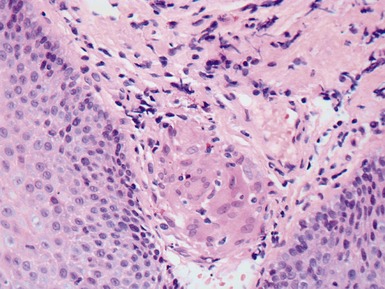
CROHN’S DISEASE OF THE ESOPHAGUS
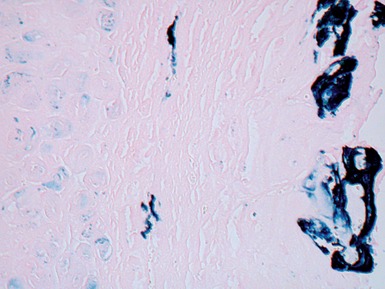
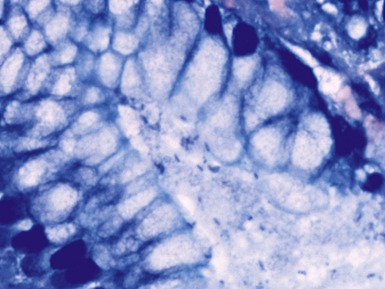
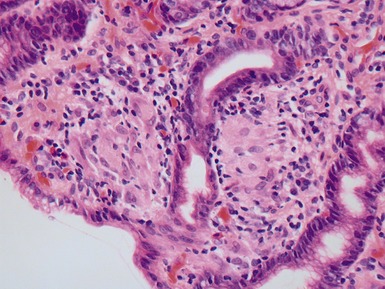
• May have well formed non-caseating epithelioid granulomas in lamina propria beneath epithelium (Fig 14.12)
STOMACH
• Endoscopic biopsies for assessment of gastritis by far the most common gastric specimen for pediatric surgical pathologists
• Other entities such as Menetrier’s disease, dysplasia, GAVE and many other specific histological lesions seen in adults are exceptionally uncommon in children and are not described here
GASTRITIS
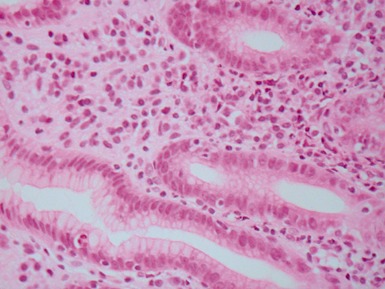
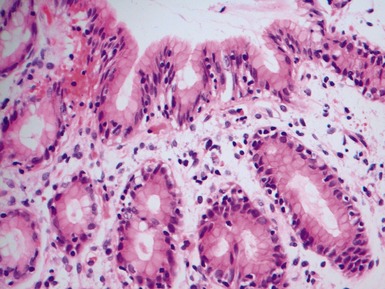
Helicobacter pylori gastritis
Crohn’s disease associated gastritis
• Presence of eosinophils in deep gastric lamina propria in pediatric gastritis is associated with Crohn’s disease
• Note that especially in children, non-specific gastritis may also be associated with ulcerative colitis
Lymphocytic gastritis
SMALL INTESTINE
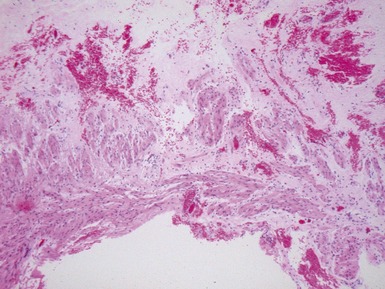
INTESTINAL ATRESIA
MECKEL’S DIVERTICULUM
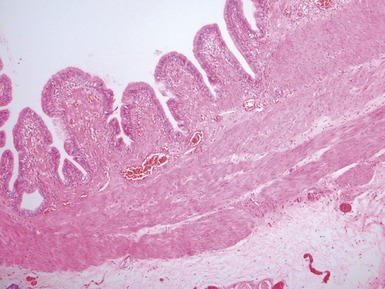
DUPLICATION CYSTS