96 Gastrointestinal Infections
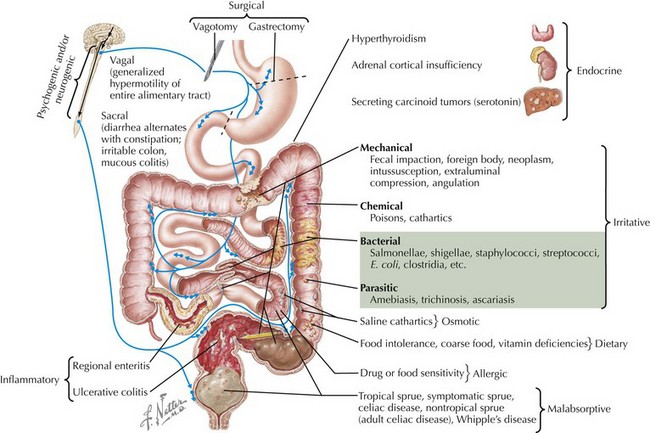
Gastrointestinal (GI) infections, particularly acute gastroenteritis, cause significant pediatric morbidity and mortality worldwide. Gastroenteritis is an infection of the GI tract characterized by vomiting, diarrhea, or both with three or more loose or watery stools a day. The worldwide mortality of diarrheal illness in children has been estimated at 1.8 million. In the United States, it is estimated that gastroenteritis primarily affects children younger than 5 years of age with 21 to 37 million episodes annually, approximately 200,000 hospitalizations, and 300 to 400 deaths per year. More readily accessible treatment has been made through the uptake of aggressive oral rehydration therapy (ORT). The causes of acute diarrhea in children differ by location, time of year, and immunologic status (Figure 96-1). This chapter discusses diarrheal illness caused by bacteria and viruses; parasites are discussed in Chapter 99. Additional infections of the GI tract are briefly addressed, including appendicitis, peritonitis, and intraabdominal abscesses.
Acute Infectious Diarrhea
Etiology and Pathophysiology
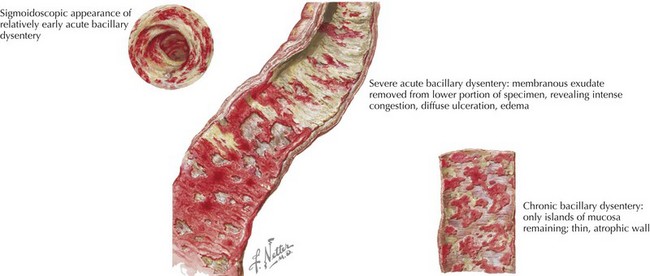
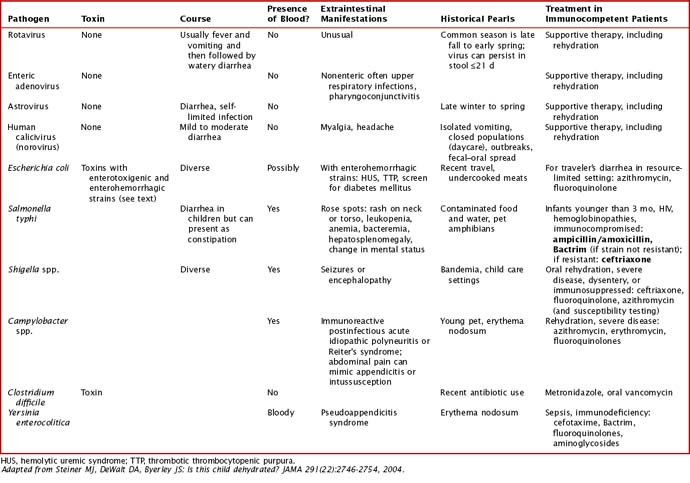
Common viral etiologies of acute infectious diarrhea in immunocompetent children include rotavirus, enteric adenoviruses, noroviruses, and astroviruses. Common bacterial pathogens include Salmonella spp., Escherichia coli, Shigella spp., and Campylobacter jejuni (Figure 96-2). Clostridium difficile is the most common cause of antibiotic-associated diarrhea, although its role in infants younger than 1 year of age is unclear. Additional causes are discussed in Table 96-1 with further discussion of treatment. These pathogens cause diarrhea by a variety of pathogenic means: (1) osmotic or malabsorptive, (3) inflammatory, and (3) toxigenic. In immunocompromised hosts, cytomegalovirus and herpes simplex virus should also be considered as causes of infectious diarrhea.
Clinical Presentation
Certain infectious agents are associated with extraintestinal manifestations. Shigella spp. organisms produce a toxin that has been associated with seizure. Yersinia enterocolitica infection has been associated with reactive arthritis. Additional extraintestinal manifestations can be seen in Table 96-1.
Evaluation and Management
A brief discussion of rehydration is provided here, but more detailed discussions can be found in the Suggested Readings section at the end of the chapter. Current recommendations from the American Academy of Pediatrics encourage use of ORT in managing acute gastroenteritis in children. Oral rehydration occurs in two phases of treatment: a rehydration phase in which water and electrolytes are given in the form of an oral rehydration solution (ORS) for existing losses and a maintenance phase. ORS introduces glucose as well as sodium at the same time to allow for coupled transport. The World Health Organization’s components for rehydration solution consist of at least a complex carbohydrate or 2% glucose and 50 to 90 m Eq/L of sodium. Early refeeding is now encouraged after previous losses are corrected. Antimicrobial therapies for certain bacterial etiologies are discussed in Table 96-1.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree