32 Gastrointestinal Disorders
The pediatric primary care provider plays an integral role in the care of children with GI dysfunction. A thorough understanding of the anatomy, physiology, and common disorders of the GI system is needed to appropriately assess and treat pediatric GI problems. This chapter focuses on pathologic GI disorders commonly seen in children. Other problems of the GI system, such as obesity, anorexia, bulimia, encopresis, and constipation, are discussed in Chapters 10, 12, and 19.
 Anatomy and Physiology
Anatomy and Physiology
Entry of feces into the rectum stimulates the defecation reflex. This reflex stretches the rectal wall, relaxes the internal anal sphincter, and thereby creates the need to defecate. If this urge is ignored, further fluid resorption occurs as the stool is retained, resulting in an increase in stool mass and dryness. Excessive stretching of the colon from the hard, dry stool bolus can lead to decreased peristalsis, further complicating the retention of stool.
 Assessment
Assessment
History
The history assesses the following:
• Family history of any GI disease (e.g., gallbladder disease, ulcers, or allergy to any food product)
• Past medical history related to the GI system (e.g., illnesses, surgeries, anatomic problems, such as cleft lip or palate, esophageal atresia)
• Feeding habits and nutrition history or current diet (what, when, how often, what tolerated)
• Presence of pain (onset, location, type, quality, aggravating and alleviating factors)
 Epigastric pain usually indicates pain from the liver, pancreas, biliary tree, stomach, and upper part of the small bowel (duodenum).
Epigastric pain usually indicates pain from the liver, pancreas, biliary tree, stomach, and upper part of the small bowel (duodenum). Periumbilical pain is generated from the distal end of the small intestine, cecum, appendix, and ascending colon.
Periumbilical pain is generated from the distal end of the small intestine, cecum, appendix, and ascending colon. Referred pain is a diagnostic challenge. For example, because of convergent nerve pathways, inflammation of the diaphragm can generate pain that is perceived as shoulder or lower neck pain. When visceral pain is overwhelming, referred pain occurs.
Referred pain is a diagnostic challenge. For example, because of convergent nerve pathways, inflammation of the diaphragm can generate pain that is perceived as shoulder or lower neck pain. When visceral pain is overwhelming, referred pain occurs. Secondary autonomic nervous system stimulation associated with acute abdominal pain can produce symptoms of sweating, nausea, vomiting, pallor, and anxiety.
Secondary autonomic nervous system stimulation associated with acute abdominal pain can produce symptoms of sweating, nausea, vomiting, pallor, and anxiety.• Bowel habits (frequency, times per week, consistency, associated pain, the need for medications or enemas)
• Constipation and diarrhea (patient’s definition of each, how often they occur, treatment tried)
• Thirst level (increased or decreased)
• Food intolerance or allergy (what foods, symptoms, treatment)
• Heartburn, belching and flatulence, vomiting
• Other signs or symptoms (e.g., apnea or asthma that may be caused by gastroesophageal reflux [GER])
Physical Examination
When assessing a suspected GI problem, a head-to-toe physical examination is indicated.
• Plot growth parameters, including weight for height, to establish proportionality of the patient and exclude certain growth aberrations from the diagnosis.
• Determine body mass index (BMI). The BMI is one of the first indicators used to assess body fat and is a common method of tracking weight problems and obesity in children 2 years and older (see Chapter 10 for more details).
• Determine hydration status (skin turgor, mucous membranes, peripheral pulses, tears, capillary filling).
• Inspect the abdomen for visible peristalsis, rashes, lesions, asymmetry, masses, enlarged organs, and pulsations.
• Auscultate for frequency of bowel sounds (normal is 5 to 20 per minute).
• Percuss for density and to measure organs.
• Palpate both lightly and deeply.
• Assess peritoneal irritation:
 Check for the obturator sign: A supine patient flexes the right thigh at the hip with the knee bent and internally rotates the hip. The sign is positive when it induces abdominal pain.
Check for the obturator sign: A supine patient flexes the right thigh at the hip with the knee bent and internally rotates the hip. The sign is positive when it induces abdominal pain. Check for the psoas sign: The patient lies on the left side and extends and then flexes the right leg at the hip. A positive sign is one that induces abdominal pain.
Check for the psoas sign: The patient lies on the left side and extends and then flexes the right leg at the hip. A positive sign is one that induces abdominal pain.• Perform a rectal examination when intraabdominal, pelvic, or perirectal disease is suspected (the newborn examination should always routinely assess for anal stenosis). Include external inspection and internal palpation for masses, stool, or irregularities. The index finger is typically used because of its increased sensitivity; however, in infants and young children, use the fifth finger. Insert a gloved, lubricated finger into the rectum. Place the other hand on the abdomen for a bimanual examination. Young pediatric patients should be supine with their feet held together and knees and hips flexed, putting their legs over their abdomen. Adolescent males can be lying on their side or standing with the hips flexed and the upper part of the body on the examination table. Adolescent females can be lying on their side or, if a concurrent pelvic examination is to be done, in the lithotomy position.
• Perform a gynecologic examination if a pathologic pelvic condition is suspected (see Chapter 35).
Common Diagnostic Studies
Laboratory tests are performed as indicated:
• Urinalysis (UA) and urine culture
• Complete blood count (CBC) with differential
• Serum chemistry screen, liver profile, lipid profile, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), thyroid function
• Stool examination for ova and parasites (O&P), culture, blood, white blood cells (WBCs), pH, reducing substances
• Fecal fat collection for 72 hours to rule out fat malabsorption
• Urine tests for gonorrhea or chlamydia, Papanicolaou (Pap) smear and vaginal cultures and/or smears if pelvic or gynecologic pathologic condition is suspected
Imaging of the abdomen may include the following (Clayton, 2010):
• Ultrasound (US)—no ionizing radiation, noninvasive, relatively inexpensive (especially for pyloric stenosis, intussusceptions, appendicitis, cholelithiasis, trauma)
• Computed tomography (CT) scan—used only after other imaging studies; quick, but invasive, increased radiation, possible sedation (helpful in nephrolithiasis, appendicitis [the gold standard], intraabdominal masses, pancreatitis)
• Magnetic resonance imaging (MRI)—noninvasive and no ionizing radiation; more costly, sedation may be required (useful in a wide range of disorders)
• Nuclear medicine (scintigraphy)—provide functional and quantifiable data (especially with biliary disease, GER, and Meckel diverticulum)
Specialized tests may also be considered:
• Duodenal aspirate to identify existing infection
• Esophageal pH probe to establish gastroesophageal reflux disease (GERD), with a pH of less than 4 representing a reflux episode
• Breath hydrogen test if lactose intolerance is suspected
• Sweat chloride test if cystic fibrosis (CF) is suspected (see Chapter 31)
 Management Strategies
Management Strategies
Medications
Many common medications are used to treat various GI disorders:
• Antibiotics, antifungals, or anthelmintics for bacterial, fungal, or parasitic infections
• Antiemetics for nausea or vomiting
• Antidiarrheals occasionally for persistent diarrhea or diarrhea associated with chronic disease, but never for acute diarrheal diseases because toxins need to be excreted from the body
• Stool softeners, laxatives, and cathartics for acute treatment and long-term management of constipation and encopresis (see Chapter 12)
• Medications that alter GI motility or tone to treat GERD
• Oral steroids, parenteral steroids, and other immunosuppressants in the treatment of inflammatory bowel disease
• Pain medication and antispasmodics in selected acute and chronic GI conditions
• Medications that alter gastric acidity to treat GERD and ulcer disease
• Iron supplementation as supportive therapy for chronic disease
Probiotics and Prebiotics
Probiotics are foods or dietary supplements with viable microorganisms that alter the microflora of the host, stimulating favorable growth and/or activity of bacteria. Prebiotics are supplements or foods with nondigestible ingredients that benefit the host by stimulating favorable growth and/or activity of probiotic bacteria. Probiotics have been studied more extensively than prebiotics, with modest effectiveness shown in the prevention of acute infectious diarrhea as well as the treatment of acute viral gastroenteritis and in the prevention of antibiotic-associated diarrhea. There is also some evidence of effectiveness in preventing necrotizing enterocolitis in low birthweight infants, and in treating Helicobacter pylori gastritis, irritable bowel syndrome, chronic ulcerative colitis, and colic. Prebiotics may be of some benefit in preventing infection in healthy infants. Though these products seem to be safe in healthy infants and children, there is some concern about the safety of administering them to high-risk children including immunocompromised, ill preterm infants, and/or children with indwelling medical devices (Thomas et al, 2010; Weng and Walker, 2006). See Chapter 42 for further information about using probiotics.
Nutrition and activity
A nutritional plan that meets the recommended daily needs should be encouraged to promote normal GI function, growth, and development. Intake of fluids to ensure hydration is equally important. Dysfunction of the GI tract can be either short term or long term and can require alterations in dietary intake. Consultation with a registered dietitian is important in designing an adequate nutritional plan for a child with a long-term GI problem (see Chapter 10 for more detail).
 Upper Gastrointestinal Tract Disorders
Upper Gastrointestinal Tract Disorders
Dysphagia
Description
Dysphagia, or difficulty swallowing, may be caused by a variety of disorders. Younger children may be unable to swallow, and older children can have awareness that something is wrong with their swallowing ability or may complain of something being stuck in their throat (globus). The physiology of swallowing is complex with oral, pharyngeal, and esophageal phases. The oral phase refers to ingestion, mastication, and the propulsion of food to the back of the mouth as a bolus. The pharyngeal phase includes the swallowing and transfer of food from the pharynx to the esophagus. Airway closure is critical during the pharyngeal phase, and the child needs to have intact motor and sensory pharyngeal protective mechanisms to prevent aspiration. The esophageal phase allows food to pass into the stomach.
Clinical Findings
Diagnostic Studies
Vomiting and Dehydration
Description
• Newborn or young infant—infectious process, congenital gastrointestinal anomaly, CNS abnormality, or inborn errors of metabolism
• Infants and young children—gastroenteritis, GERD, milk/soy protein allergies, pyloric stenosis or obstructive lesion, inborn errors of metabolism, intussusception, child abuse, intracranial mass lesion
• Older children and adolescents—gastroenteritis, systemic illness, CNS (cyclic vomiting syndrome [CVS], abdominal migraine, meningitis, brain tumor), intussusception, rumination, superior mesenteric artery syndrome, pregnancy
Epidemiology
Vomiting
Following is a list of potential causes of vomiting by site of origin:
• Oropharynx: Cleft palate and laryngopharyngeal cleft
• Upper GI: Congenital stricture, foreign body, gastritis and/or esophagitis, gastric web, pyloric stenosis, tracheoesophageal fistula, vascular ring, peptic ulcer disease (PUD)
• Small intestine: Annular pancreas, choledochal cyst, intestinal atresias and stenosis, intestinal malrotation with volvulus, intestinal pseudo-obstruction
• Colon: Hirschsprung disease, intussusception, meconium ileus, necrotizing enterocolitis, fecal impaction
• Hepatobiliary or pancreatic dysfunction
• Infections: Bacterial enteritis, otitis media, sepsis, urinary tract infection (UTI), viral gastroenteritis (VGE), hepatitis
• Neurologic: Congenital anatomic malformation, gray and white matter degenerative disorders, hydrocephalus, kernicterus, brain tumors, migraine headache, head trauma
• Other: Cow’s-milk protein allergy (CMP intolerance), inborn errors of metabolism, maternal drug exposure and/or withdrawal, toxic ingestions, appendicitis, cyclic vomiting, pneumonia, drug or alcohol ingestion, eating disorders, pregnancy
Clinical Findings
History
The vomiting history should assess the following:
• History of illnesses, surgeries, or hospitalizations
• Medications currently being taken (including over-the-counter, herbal, cultural, and homeopathic remedies)
• Recent exposure to illness, injury, or stress; recent travel (including camping); swimming activities
• Family history of GI disease or fetal or neonatal deaths (metabolic syndrome, congenital anomaly)
• Onset and duration of vomiting, quality and quantity, presence of blood or bile, odor, precipitating event
• Relationship of vomiting to meals, time of day, or activities
• Vomiting early in the morning
• Presence of associated symptoms: Diarrhea, fever, ear pain, UTI symptoms, vision changes, cough, headache, seizures, high-pitched cry, polydipsia, polyuria, polyphagia, anorexia
The dehydration history should assess the following:
Physical Examination
• Growth parameters and vital signs
• Neurologic examination: Nuchal rigidity, decreased level of consciousness, and behavioral changes, which can include irritability or lethargy. Sensorium remains intact until there is greater than 6% of weight loss as a result of dehydration. Hypotension is a late manifestation of dehydration.
• Abdominal examination: Inspect for distention, abdominal scars from previous surgery (may be associated with obstruction and/or adhesions), or visible peristaltic waves. Auscultate bowel sounds (i.e., increased with gastroenteritis, decreased with obstruction, absent with ileus or peritonitis). Palpate the abdomen for pain and/or rebound tenderness. Assess abdominal organs (liver and spleen size, masses). Perform a rectal examination as indicated.
• Respiratory examination: Tachypnea, decreased oxygen saturation, stridor
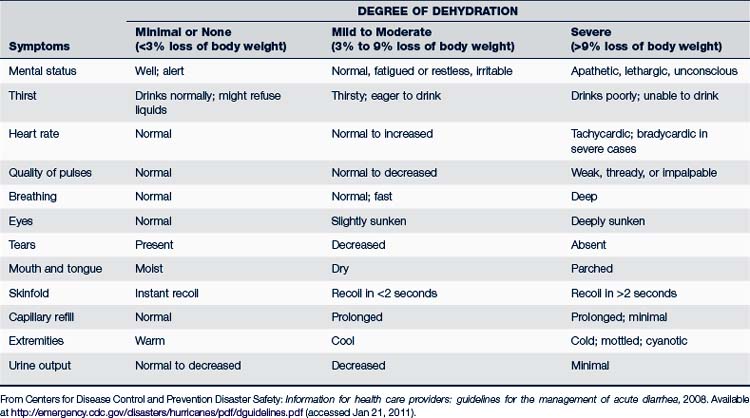
• Assessment of dehydration (Table 32-1)
 One of the most useful clinical signs of hydration is capillary refill time (CRT). Normal CRT is less than 2 seconds. CRT, skin turgor, and tachypnea, considered together, are most helpful in determining dehydration (Steiner et al, 2004).
One of the most useful clinical signs of hydration is capillary refill time (CRT). Normal CRT is less than 2 seconds. CRT, skin turgor, and tachypnea, considered together, are most helpful in determining dehydration (Steiner et al, 2004). A clinical dehydration scale (CDS) is a predictive tool regarding length of stay and need for intravenous fluids (Goldman et al, 2008). The four parameters used for assessment are general appearance, eyes (sunken or not), moistness of mucous membranes, and presence of tears.
A clinical dehydration scale (CDS) is a predictive tool regarding length of stay and need for intravenous fluids (Goldman et al, 2008). The four parameters used for assessment are general appearance, eyes (sunken or not), moistness of mucous membranes, and presence of tears. Mahajan (2009) provides five points to assess the level of dehydration: volume deficit with history and physical, osmolar disturbance (serum sodium and osmolality), acid-base disturbance (blood pH, Pco2, serum bicarbonate), potassium, and renal function (blood urea nitrogen [BUN]), creatinine, urine specific gravity.
Mahajan (2009) provides five points to assess the level of dehydration: volume deficit with history and physical, osmolar disturbance (serum sodium and osmolality), acid-base disturbance (blood pH, Pco2, serum bicarbonate), potassium, and renal function (blood urea nitrogen [BUN]), creatinine, urine specific gravity.Diagnostic Studies
Diagnostic studies are performed as indicated by the probable diagnosis:
• Complete blood count (CBC) with differential, blood culture
• Electrolytes, including BUN and creatinine, glucose, and liver function tests
 Serum bicarbonate less than 17 mEq/L (differentiates mild from moderate/severe hypovolemia) (Mahajan, 2009)
Serum bicarbonate less than 17 mEq/L (differentiates mild from moderate/severe hypovolemia) (Mahajan, 2009)• Serum lactate, organic acids, ammonia for metabolic disorders (may only be abnormal during episodes of vomiting)
• Stool for culture and occult blood, leukocytes, parasites, fat, pH, reducing substances
• Rapid strep test and/or throat culture
• Abdominal radiographs (suspected obstruction or foreign body ingestion, organomegaly, or a palpable mass)
• Chest radiograph (suspected pneumonia)
• US (abscesses, masses, stenoses, cysts, appendicitis, pyloric stenosis)
• Barium swallow or enema (malrotation, pyloric stenosis, GER, masses)
• Endoscopy (obstruction, hemorrhage, infection; collect biopsies)
• Esophageal pH probe analysis, scintiscan
• CT scan or MRI to diagnose masses, inflammation, herniations, perforations, and obstructions
Differential Diagnosis
TABLE 32-2 Differential Diagnosis of Vomiting in Infants and Children
| Infant | Child | Adolescent |
|---|---|---|
| Common Conditions | ||
| Gastroenteritis | Gastroenteritis | Gastroenteritis |
| GERD | GERD | GERD |
| Overfeeding | Gastritis | Gastritis |
| Anatomic obstruction: pyloric stenosis, malrotation with intermittent volvulus, intestinal duplication, Hirschsprung disease, antral/duodenal web, foreign body, or incarcerated hernia | Toxic ingestion: lead, iron, or vitamins A and D | Toxic ingestion |
| Systemic infection: UTI, pneumonia, hepatitis | Systemic infection: UTI or pyelonephritis; pneumonia; hepatitis | Systemic infection |
| Pertussis syndrome | Pertussis syndrome | Pertussis syndrome |
| Otitis media | Otitis media, sinusitis | Sinusitis |
| Appendicitis, small bowel obstructionMigraineMedication: ipecac, digoxin, theophylline, etc. | Appendicitis, small bowel obstruction, IBD | |
| Migraine | ||
| Medication: ipecac abuse/bulimia | ||
| Pregnancy, PID | ||
| Rare Conditions | ||
GERD, Gastroesophageal reflux disease; IBD, inflammatory bowel disease; PID, pelvic inflammatory disease; UTI, urinary tract infection.
Adapted from Blanchard S, Czinn S: Peptic ulcer disease in children. In Kliegman RM, Behrman RE, Jenson HB et al: Nelson textbook of pediatrics, ed 18, Philadelphia, 2007, Saunders, pp 1572-1574; Vandenplas Y, Rudolph C, Di Lorenzo C, et al: Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN), J Pediatr Gastroenterol Nutr 49(4):498-547, 2009. Used with permission of Lippincott Williams & Wilkins.
Management
Vomiting
• Identify and alleviate the cause as soon as possible.
• Antiemetics, though not recommended in acute gastroenteritis, or when cause is unknown, may at times be warranted. Newer medications such as 5-HT3 receptor antagonists (ondansetron or granisetron) do not have adverse effects on the CNS and may be indicated in older children (Chandran and Chitkara, 2008; Ulshen, 2009).
• Refer to specialist for persistent vomiting, recurrent vomiting, or vomiting associated with significant underlying process.
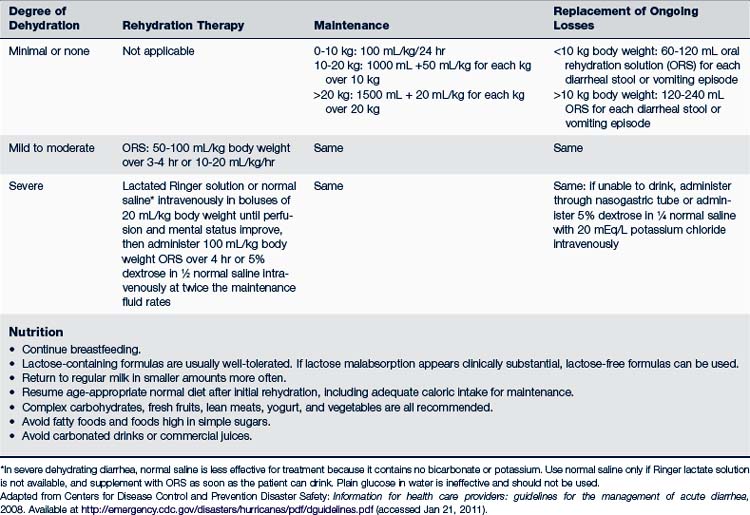
Dehydration
• Determine the degree of dehydration.
 If minimal, mild, or moderate, oral rehydration solution (ORS) with 70 to 90 mEq/L sodium, 25 g/L glucose, 20 mEq/L potassium, 30 mEq/L base (in the form of citrate, acetate, or lactate) with a defined osmolarity of 240 to 300 mOsm/L is recommended.
If minimal, mild, or moderate, oral rehydration solution (ORS) with 70 to 90 mEq/L sodium, 25 g/L glucose, 20 mEq/L potassium, 30 mEq/L base (in the form of citrate, acetate, or lactate) with a defined osmolarity of 240 to 300 mOsm/L is recommended. Pediatric subcutaneous rehydration using recombinant human hyaluronidase is an alternate method, effective when used in children with mild to moderate dehydration who require parenteral therapy (Allen et al, 2009).
Pediatric subcutaneous rehydration using recombinant human hyaluronidase is an alternate method, effective when used in children with mild to moderate dehydration who require parenteral therapy (Allen et al, 2009).• Initial rehydration, maintenance of fluids, and replacement of ongoing losses are stages of treatment (Table 32-3). Physiologically sodium and glucose are coupled in transport across the intestinal brush border into systemic circulation to maximize rehydration. Administration of fluid should be in frequent, small (5 mL or less) amounts. Larger amounts may be given as tolerated. Plain water, juices, soda, milk, and sports drinks should be avoided because these liquids are hyperosmolar and do not provide appropriate replacement of sugars and electrolytes. A pediatric emergency department using ORS in children with moderate dehydration showed not only successful rehydration, but also a decreased length of stay, less staff use, and more satisfied parents (Bell, 2010). Palatability of ORS does not affect the quantity consumed (Freedman et al, 2010). Homemade solutions can be used when premade ORS is not available (see http://rehydrate.org). Refeeding should resume as quickly as possible because the gut needs nutrition to facilitate mucosal repair following injury.
• Antiemetics. A single dose of an oral disintegrating tablet of ondansetron (2 mg for children 8 to 15 kg, 4 mg for children 15 to 30 kg, and 8 mg for more than 30 kg) reduces vomiting, decreases the chance of dehydration, and increases the success of oral hydration (Amir, 2007; Freedman et al, 2006; Roslund et al, 2006).
• Refer if the child has a toxic appearance, severe dehydration, projectile vomiting, abnormal examination, vomiting for greater than 12 hours, or vomiting of blood, bile, or fecal matter, or significantly decreased urine output.
Cyclic Vomiting Syndrome
Description
CVS is characterized by recurrent, discrete, self-limited episodes of vomiting between which are completely symptom-free periods. CVS is often associated with abdominal migraines (discussed on p 765). During episodes there is intense nausea and unremitting vomiting (a median of six times per hour at peak) often with bilious emesis (83%) and severe abdominal pain (80%) (Li et al, 2008). Accompanying symptoms include pallor, listlessness, anorexia, nausea, retching, abdominal pain, headache, and photophobia. The periods of vomiting may last hours or even days; the symptom-free periods may last for weeks or even years. Consensus criteria for CVS have been established for diagnosis (see www.naspghan.org).
Epidemiology
The etiology of CVS is unknown, but there is a link with migraines. Cyclic vomiting may occur any time between infancy and young adulthood, most commonly diagnosed between 3 and 7 years old. Girls are affected more often than boys (60:40), as are Caucasian, elementary school–age children. Affected individuals tend to have mothers and maternal grandmothers who have a higher incidence of migraine headaches, depression, anxiety, irritable bowel syndrome (IBS), and hypothyroidism (Boles et al, 2005; Li et al, 2008). CVS is often a precursor of later classic migraines.
Clinical Findings
History
• Red flags have been identified (Box 32-1)
• Family history positive for migraine headache is common
• A prodromal period (some combination of pallor, anorexia, nausea, abdominal pain, or lethargy) and/or a recovery period (from ill to playing again) that is brief
• Episodes that begin and end abruptly
• Episodes more likely to occur early in the morning (3:00 to 4:00 am) or on awakening
• An identifiable trigger is commonly seen in children—physical stress (infection, lack of sleep, menstrual periods) or psychological stress (birthdays, holidays, school-related), or food products (e.g., chocolate, cheese, monosodium glutamate)
• Intense nausea not relieved by vomiting
• Headache, motion sickness, photophobia, phonophobia, or vertigo may occur
BOX 32-1 Red Flags of Cyclic Vomiting Syndrome
• Abdominal signs (e.g., bilious vomiting, abdominal tenderness, and/or severe abdominal pain, hematemesis)
• Triggering events (e.g., fasting, high-protein meal, or intercurrent illness)
• Abnormal neurologic examination (e.g., severely altered mental status, abnormal eye movements, papilledema, motor asymmetry, and/or gait abnormality [ataxia])
• Progressively worsening episodes or conversion to a continuous or chronic pattern
Differential Diagnosis
CVS is a diagnosis of exclusion. Severe GI symptoms can indicate hydronephrosis, cholelithiasis, pancreatic disease, or ureteropelvic junction. CVS precipitated by concurrent illness, fasting, or high-protein meals can indicate a metabolic disorder. An abnormal neurologic examination is suggestive of increased intracranial pressure. Approximately 10% of children with CVS-like history have a specific underlying disorder. Although uncommon, Munchausen by proxy syndrome has been known to mimic CVS in a child given ipecac (Li et al, 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree