CHOLELITHIASIS
Epidemiology
• 10–15% prevalence in adults overall; 1–3% of pregnant women
• Risk factors: Preg (impaired gallbladder emptying, increased biliary sludge); ↑ estrogen (gender [ 2× >
2× >  ], obesity, rapid weight loss, Preg); ethnicity (75% of Native Americans); age (>40 y); drugs (OCPs, estrogen, clofibrate, octreotide, ceftriaxone, TPN); bile acid metabolism disorders; hyperlipidemia syndromes (↑ biliary cholesterol secretion & cholesterol sat of bile)
], obesity, rapid weight loss, Preg); ethnicity (75% of Native Americans); age (>40 y); drugs (OCPs, estrogen, clofibrate, octreotide, ceftriaxone, TPN); bile acid metabolism disorders; hyperlipidemia syndromes (↑ biliary cholesterol secretion & cholesterol sat of bile)
Pathophysiology
• Bile = pathway for elimination of excess cholesterol either as free cholesterol or as bile salts; cholesterol-saturated bile → crystal formation → bile stasis → aggregation
• Types of stones: Mixed; cholesterol (up to 80% of gallstones, up to 80% radiolucent); black pigments (unconjugated bilirubin + calcium, sterile; radiopaque); brown pigments (calcium soaps, infected ducts; radiolucent)
Clinical Manifestations
• 70–80% asymptomatic; biliary colic = acute episodic RUQ or epigastric abdominal pain radiates to right scapula or shoulder; typically resolves w/i hours; a/w nausea ± emesis; precipitated by fatty food; often nocturnal; sev includes perforation, fistulae, pancreatitis, obstructive jaundice
• Physical exam: Afebrile, ± RUQ tenderness or epigastric pain
Workup
• RUQ US: Mobile echogenic focus w/ acoustic shadow; sens & spec >95% for gallstones >1.5 mm in diameter
• Labs: AST, ALT, Amy, lipase, CBC
Treatment of Symptomatic Cholelithiasis
• Initial medical mgmt: IVF, analgesia, NG suction (rare), no Abx for cholelithiasis w/o infxn/cholecystitis
• Cholecystectomy if symptomatic: Failed medical mgmt, ascending cholangitis, common bile duct obst, pancreatitis. 36% pregnant women initially managed conservatively → Surg (Glasgow Surg Endosc 1998;12: 241). Prophylactic cholecystectomy only if large stones or ↑ risk gallbladder cancer.
• For poor surgical candidates: Oral dissolution rx (ursodiol); extracorporeal shock wave lithotripsy for mild, uncomp biliary colic (contraindicated in Preg)
CHOLECYSTITIS
Definition and Epidemiology
• Inflammation of the gallbladder: Acute (rapid onset, gallstone obst); chronic (transient obst → low-grade inflammation/fibrosis); acalculous (inflammation w/o obst)
•  >>
>>  due to estrogen (↑ cholesterol secretion) & progesterone (↓ bile acid secretion & ↑ stasis)
due to estrogen (↑ cholesterol secretion) & progesterone (↓ bile acid secretion & ↑ stasis)
• 1:1600 to 1/10000 pregnancies; 2nd most common cause of Surg during Preg
Pathophysiology
• >90% due to cystic duct stone → inflammation
• Gallbladder stasis/ischemia → acalculous cholecystitis; in sev injury, major nonbiliary Surg, sev trauma, burns, sepsis, infxn (CMV, crypto, HIV), vasculitis (polyarteritis nodosa)
Clinical Manifestations
• Similar to acute cholelithiasis, but steady and sev w/ RUQ/epigastric pain; tenderness, fever, nausea, ± emesis
• Physical exam: RUQ tenderness, Murphy sign (increased RUQ pain & insp arrest w/ R subcostal palpation), guarding/rebound, 15% palpable gallbladder
• Acalculous cholecystitis: Unexplained fever or RUQ pain w/i 2–4 w of major Surg; critically ill pt w/ prolonged NPO; multiorgan failure
Workup
• Labs: ↑ WBC ± ↑ bilirubin, mild ↑ AST/ALT, ± mod ↑ Amy (if vomiting)
• Abdominal XR: Radiopaque stones in 15%
• RUQ US: Gallbladder wall thickening, pericholecystic fluid, sono Murphy sign
• MRI in Preg if RUQ sono nondiagnostic; dilated common bile duct = choledocholithiasis
• HIDA scan (99m Tc hepatobiliary imaging): Most sensitive if bilirubin <5 mg (98% sens & 81% spec); demonstrates an obstructed cystic duct
Treatment
• NPO, IVF, NGT if intractable vomiting, analgesia
• IV Abx (2nd or 3rd gen cephalosporin + metronidazole; fluoroquinolone + metronidazole for sev cases)
• Cholecystectomy – laparoscopic, w/i 2–4 d after admission; cholecystostomy or percutaneous drainage if too ill for Surg. Surg in Preg may be more difficult, but may ↓ morbidity; perform in 2nd trimester if poss (Surg Endosc 2010;24:108).
APPENDICITIS
Definition and Epidemiology
• Inflammation of appendiceal wall → ischemia or perforation
• Most common nontraumatic surgical emergency during Preg; 1:1600 pregnancies; usually in 2nd trimester
• Peak incid in 2nd & 3rd decades of life; rare at extremes of age
• Incid much lower in developing countries & in lower socioeconomic groups
• Morbidity & mortality often higher in Preg due to delay in dx
Pathophysiology
• Appendiceal luminal obst (50–80%) usually by fecalith (accumulated/hardened fecal matter around vegetable fibers) → inflammation/distention/ulceration/rupture. Other causes: Lymphadenitis (viral infections), inspissated barium, parasites (eg, pinworm, Ascaris, Taenia), & tumors (eg, carcinoid or carcinoma).
• Visceral pain poorly localizes to periumbilical or epigastric region; spread of peritoneal inflammation eventually localizes to RLQ
Clinical Manifestations
• Vague periumbilical or RLQ pain, anorexia, nausea, vomiting, low-grade fever
• In Preg appendix displaced by gravid uterus → RUQ pain possible
• Tender McBurney point = 1⁄³ distance from anterior-superior iliac spine & umbilicus; psoas sign = pain w/ right hip flexion; Rovsing sign = LLQ palpation elicits RLQ pain; referred rebound tenderness often absent early & in Preg
• Temperature >38.3°C (101°F) & rigidity suggest perforation
• ↑ abortion or PTL risk; no impact on fertility unless ruptured appendix w/ subseq adhesive dz
Workup
• Labs: Mod leukocytosis (not helpful in Preg), elevated CRP/ESR
• US (1st-line in Preg) = enlarged thick-walled appendix; useful to exclude ovarian cysts, ectopic Preg, or tuboovarian abscess
• Contrast-enhanced or nonenhanced abdominal CT (gold std in nonpregnant pts): Distended, noncontrast-filled appendix, thickened appendiceal wall w/ periappendiceal stranding & often the presence of a fecalith (PPV 95–97%, overall accuracy 90–98%). MRI preferred in Preg.
Treatment and Medications
• Electrolyte correction & IVF
• Perioperative Abx: Broad coverage for gram-positive/negative & anaerobes (2nd gen cephalosporin + metronidazole or clindamycin). Conservative mgmt w/ antibiotic alone may be successful in some nonpregnant pts (BMJ 2012;344:e2156).
• Immediate appendectomy (laparoscopic preferred, safe during all trimesters of Preg)
PANCREATITIS
Definition and Etiology (Acute Pancreatitis)
• Inflammation of the pancreas; diagnosed w/ 2 of the following criteria: Characteristic abdominal pain, elevation of Amy/lipase greater than 3× upper limit of nml, CT evid of acute pancreatitis
• Incid ∼0.1% in Preg
• Consider: Gallstones, EtOH use, meds, hypertriglyceridemia, HyperCa, Pancr neoplasm or trauma. Consider dx if pain, N/V in pts after upper abd procedures, eg, splenectomy.
Clinical Manifestations
• Periumbilical or epigastric pain radiating to the back; nausea, vomiting, fever
• Life-threatening complication of AFLP (Am J Obstet Gynecol 2004;190(2):502)
Workup
• Detailed Hx for etiology; lab: Electrolytes, Amy, lipase, triglycerides, WBC
• Abd US. CT if no etiology identified.
• Severity best assessed by APACHE II criteria (www.mdcalc.com/apache-ii-score-for-icu-mortality/)
Treatment
• NPO, IV hydration, electrolyte replacement. NG suction if persistent N/V.
• Cholecystectomy ± ERCP if secondary to gallstones
Chronic Pancreatitis
• Primary cause is alcoholism, less likely hereditary, CF, stones
• Permanent fibrotic damage to pancreas from obst of ducts
• Sx include pain, recurrent acute pancreatitis, steatorrhea, gluc intolerance
• Complications include diabetes, pseudocysts, splenic vein thrombosis
• Rx is supportive/symptomatic
IRRITABLE BOWEL SYNDROME (IBS)
Definitions
• Functional bowel d/o characterized by abdominal pain or discomfort & altered bowel habits in the absence of detectable structural abnormalities
Epidemiology
• 10–20% adults & adolescents affected worldwide w/ female predominance (2–3× >men)
• Most present w/ 1st sx before age 45
Pathophysiology (Gastroenterol Clin North Am 2003;32:385)
• Altered gut motility. Visceral hypersensitivity to stimuli. Abn CNS modulation.
• Proposed mechanisms include visceral hypersensitivity in which pt has increased motor reactivity of colon & small bowel to variety of stimuli w/ lowered sensation threshold
• Intestinal infxn, psychological or emotional stress may be triggers
Clinical Manifestations
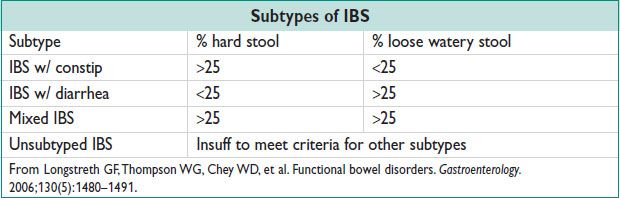
• Rome Criteria (Gastroenterology 2006;130(5):1480): Recurrent abdominal pain or discomfort at least 3 d/mo in the last 3 mo a/w 2 or more of the following:
• Improv w/ defecation
• Onset a/w a change in frequency of stool
• Onset a/w a change in appearance of stool
• Supportive sx (not diagnostic): Defecation straining, urgency or tenesmus, passing mucus & bloating, alternating bowel habits (constip alternating w/ diarrhea), dyspepsia, heartburn, nausea, & vomiting
• Location of abdominal pain variable, frequently episodic & crampy & often exacerbated by eating, emotional stress or premenstrual sx; often improved by passage of stool or flatus
Diagnostic Workup/Studies
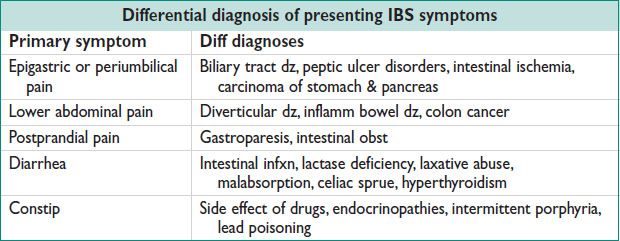
• Dx based on clinical presentation; diff dependent on location of sx
• Studies to rule out other etiologies dependent on pt sx & presentation
• Workup can include CBC, endoscopy, stool specimens (O&P) for those w/ diarrhea
• Avoid food precipitants (common triggers include coffee, disaccharides, legumes, cabbage, artificial sweeteners)
• High-fiber diets & bulking agents (may have no benefit)
• Increased physical activity & psychosocial therapy
• Diarrhea → antispasmodics, loperamide as needed
• Constip → psyllium, methylcellulose, calcium polycarbophil, lactulose, polyethylene glycol, lubiprostone, magnesium hydroxide
• Abdominal pain → smooth-muscle relaxant, TCA, SSRI
INFLAMMATORY BOWEL DISEASE
Definitions
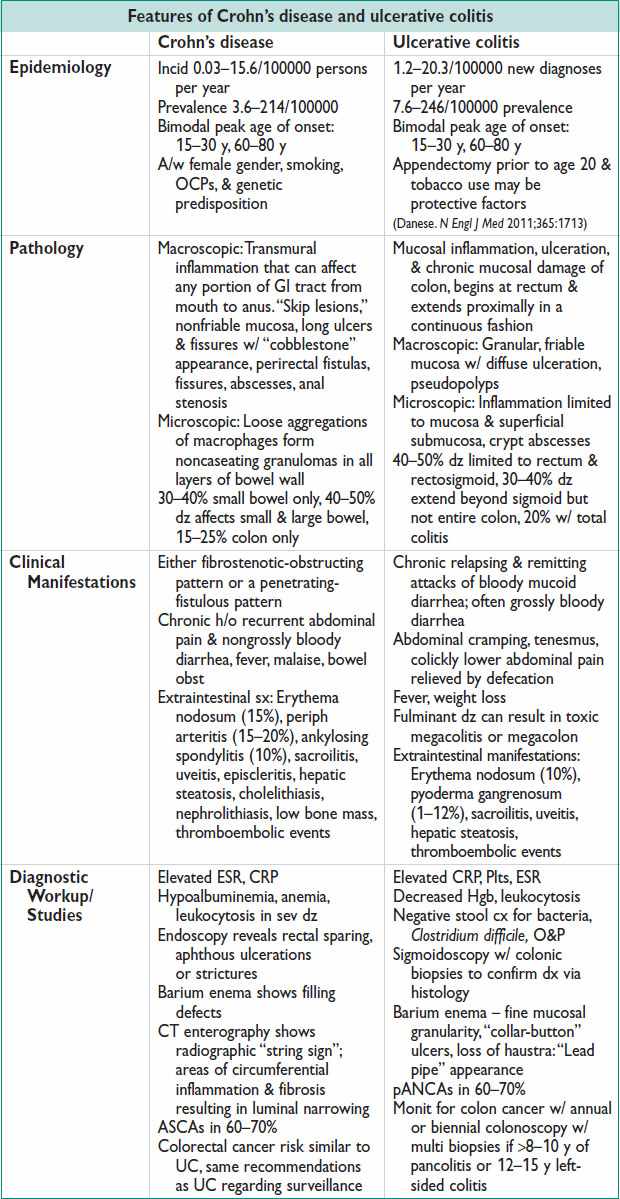
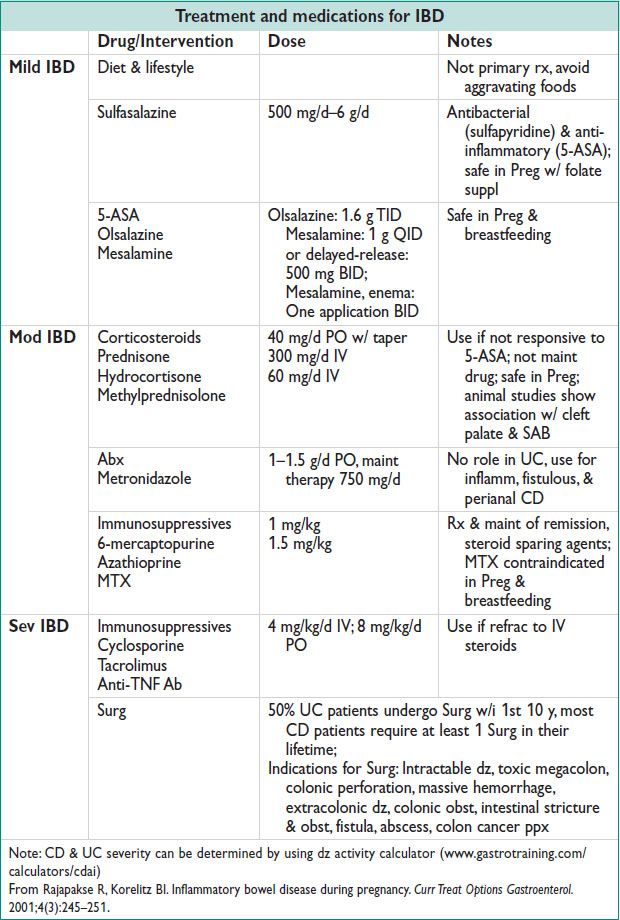
• Immune-mediated, noninfectious, chronic intestinal inflammation
• Ulcerative colitis (UC): Idiopathic continuous inflammation of colonic mucosa
• Crohn’s disease (CD): Idiopathic granulomatous transmural inflammation of GI tract, from mouth to anus, w/ skip lesions
Etiology
• Multifactorial; theoretically a chronic state of dysregulated mucosal immune fxn that is further modified by specific environmental factors (eg, smoking)
IBD and Pregnancy
• Preg does not ↑ likelihood of IBD flare
• Calcium suppl to combat osteoporosis risk
• Quiescent IBD: Nml fertility rates however fallopian tubes can be scarred by the inflamm process of CD (esp on the right)
• SAB, preterm birth, low birth weight, fetal growth restriction, & developmental defects ↑ w/ increased dz activity in CD
Effect on Preg correlates w/ dz activity at conception
Recommend pt to be in remission for 6 mo prior to conception
• Cesarean recommended only for sev anorectal & perirectal abscesses & fistulas. Reduces likelihood of fistula dev or extension into episiotomy scar.
VIRAL HEPATITIS
Clinical Manifestations
• Sx of acute hepatitis: Anorexia, nausea & vomiting, fatigue, malaise, arthralgias, myalgias, HA, photophobia, pharyngitis, cough, coryza 1–2 w prior to jaundice
Low-grade fever more common in HAV & HEV
• Dark urine & clay-colored stools may occur 1–5 d prior to onset of jaundice
• Jaundice w/ enlarged & tender liver w/ RUQ pain
• Splenomegaly & cervical adenopathy 10–20%
• During “recovery phase,” constitutional sx resolve but liver enlargement & abn liver enzymes may persist for 2–12 w
Diagnostic Labs/Exams
• Elevated AST & ALT (40–4000 U/L). Elevated bilirubin (jaundice visible when serum bilirubin >2.5 mg/dL [typically 5–20 mg/dL]). Assess PT/PTT, albumin, gluc.
Hepatitis A
• Nonenveloped RNA picornavirus. Replication limited to liver, but virus present in liver, bile, stools, & bld.
• Prevalence increases as a fxn of age & decreasing socioeconomic status
• Transmission: Fecal–oral route. 15–45-d incubation period, mean 4 w
• Dx: Active infxn = anti-HAV IgM (can persist for several months)
Prior exposure = anti-HAV IgG, detectable indefinitely → protective
• Rx: Supportive, recovery w/i 4–6 w
• No evid that HAV is teratogenic; transmission to fetus has not been reported
Hepatitis B
• Small, circular DNA hepadnavirus
• Prevalence increases w/ lower socioeconomic status, older age groups, & persons w/ risk for exposure to bld
• Acute HBV occur in 1–2/1000 pregnancies; chronic HBV occur in 5–15/1000 pregnancies
• Transmission: Bld, sexual, perinatal (esp in infants born to HBsAg carrier mothers or mothers w/ active infxn, transmission correlates w/ presence of HBeAg). 30–180-d incubation period, mean 8–12 w.
• 85–90% complete resolution of infxn after acute phase, 10–15% chronic infxn
• Chronic HBV may develop cirrhosis, fulminant liver failure, & increased risk for hepatocellular carcinoma
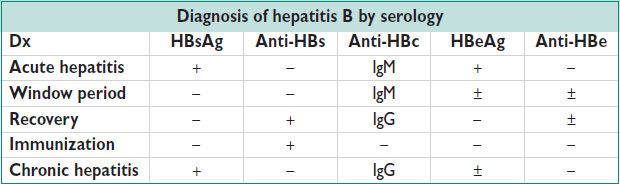
• Dx-Serology
HBsAg: 1st detectable marker, before LFTs or sx, acute or chronic infxn
Anti-HBs: Detectable indefinitely after disappearance of HBsAg or after Vz
HBcAg: Not typically detectable in serum
Anti-HBc: Present 1–2 w after HBsAg, may be only serologic marker during “window” period; anti-HBc IgM sugg acute infxn
HBeAg: Increases w/ infectivity
• Prevention: 3-dose pre-exposure vaccinations (at 0, 1, 6 mo)
HBIg postexposure ppx (including sexual exposure, needle stick, newborns)
• Rx: Acute HBV → supportive. Chronic HBV → IFN-α, lamivudine, adefovir dipivoxil, pegylated IFN, entecavir
• HBV in Preg
Routine screening at 1st prenatal visit
Increased risk of PTB, transplacental infxn uncommon, not teratogenic
Most neonat infxn vertically transmitted by peripartum exposure
High perinatal transmission rate. 30% in HBeAg (−) mothers; >85% in HBeAg (+) mothers (N Engl J Med 1975;292(15):771)
Cesarean deliv & bottlefeeding does not lower risk of transmission
Hepatitis C
• RNA virus; in US 70% genotype 1 (& most common worldwide), 30% genotype 2 or 3
1–5% prevalence in Preg, highest rates in urban populations
• Transmission: Bld exposure; 15–160-d incubation period, mean 7 w
• ∼20% chronic HCV lead to chronic active hepatitis or cirrhosis, increased risk of hepatocellular carcinoma
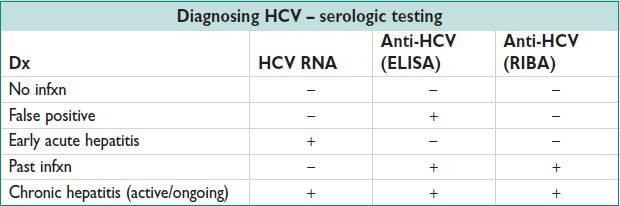
• Serology
HCV antigens not detectable in serum ∴ difficult to diagnose acute HCV
Anti-HCV (ELISA) positive in 6 w–6 mo, does not imply recovery
If + Anti-HCV, use HCV RIBA or HCV RNA (via PCR) to confirm dx
• Rx: Pegylated IFN, ribavirin
• HCV in Preg
Prenatal screening in high-risk women (concurrent alcoholism, IVDU, coexisting HIV infxn, prior bld xfusion, tattoos)
May be a/w low birth weight, need for assisted ventilation, NICU admit (Am J Obstet Gynecol 2008;199(1):38.e1)
Unclear effect on progression of hepatic fibrosis
Vertical transmission 5–10%. 3× higher w/ HIV coinfection (Lancet 1995;345(8945):289)
Risk for vertical transmission increases w/ viral load. Cesarean deliv does not ↓ risk of transmission. Prolonged rupture of membranes may ↑ transmission.
Ribavirin contraindicated in Preg. Breastfeeding not contraindicated.
Hepatitis D
• Defective RNA virus that requires coinfection or superinfection w/ HBV for replication & expression. In nonendemic areas, HDV infxn confined to persons exposed frequently to bld (IVDUs, hemophiliacs). In endemic areas, HDV infxn predominantly by nonpercutaneous means.
• Transmission: Bld, sexual. 30–180-d incubation period, mean 8–12 w
• Dx: Anti-HDV, HDV RNA
No screening indicated as counseling & rx same as HBV
May consider screening if w/ symptomatic HBV
• Rx: Similar to HBV
Hepatitis E
• RNA virus common to India, Asia, Africa, & Central America
• Transmission: Fecal–oral, rarely secondary person-to-person spread
14–60-d incubation period, mean 5–6 w
• Dx: IgM anti-HEV
• Rx: Supportive
• Fatality rate 1–2% & up to 10–20% in pregnant women
• Can cause fetal/neonat hepatitis
Prevention/Vaccinations
• HAV & HBV Vz safe during Preg. Vaccinate high-risk pts (more than 1 sex partner during prev 6 mo, treated for an STI, recent or current IVDU, having had an HBsAG-positive sex partner). May be vaccinated during Preg.
INTRAHEPATIC CHOLESTASIS OF PREGNANCY (ICP)
Definitions and Epidemiology
• Dz of intrahepatic biliary tree or hepatocellular secretory system resulting in elevated bilirubin & other solutes eliminated in bile (bile salts & cholesterol) that occurs during Preg
• 0.1–0.2% incid in North America
• Chronic hepatitis C a/w 20-fold ↑ in incid of cholestasis
Pathophysiology
• Unk but likely genetically susceptible alterations in steroid & bile acid metabolism
• HLA-B8 & HLA-BW16 & gene mutations in hepatocellular transport systems (MDR3)
• May be related to circulating estrogen levels (incid in twin pregnancies > singletons)
• Bile acids incompletely cleared & accumulate in plasma w/ assoc dyslipidemia
• ↑ mec & intrapartum fetal distress (22–41%), preterm birth (19–60%), & fetal demise (0.75–1.6%); esp if bile acids >40 μmol/L (Glantz. Hepatology 2004;467)
Clinical Manifestations and Physical Exam
• Generalized pruritus in 2nd or 3rd trimester esp on palms & soles of feet
• Jaundice (20–75%)
• No assoc rash, but excoriations from scratching
Diagnostic Workup/Studies
• Pruritus precedes lab abnormalities by several weeks
Hyperbilirubinemia (rarely exceeds 4–5 mg/dL)
↑ serum bile acids (chenodeoxycholic acid, deoxycholic acid, cholic acid) > 10 μmol/L
↑ alk phos more than nml Preg
Nml to moderately ↑ AST/ALT but seldom >250 U/L
• Liver bx shows mild cholestasis w/ centrilobular dilation w/ bile plugs (rare to bx)
• Rule out preeclampsia, not likely in setting of nml pressures & absence of proteinuria
• RUQ US to rule out cholelithiasis & biliary obst
Treatment and Medications
• Sx & labs nml 2–4 w after deliv but likely to recur in subseq pregnancies or w/ exogenous estrogen use
• Antihistamines & topical emollients for symptomatic relief of pruritus
• Ursodeoxycholic acid (probably superior rx), cholestyramine, naltrexone
• Consider antepartum testing after dx; consider deliv at 37–38 w
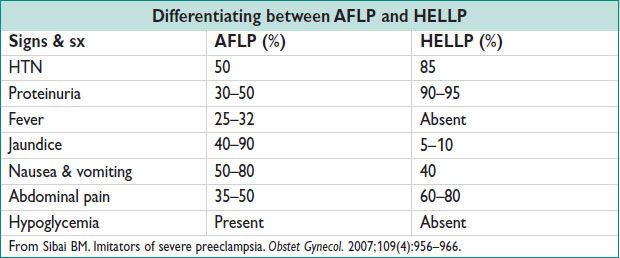
HELLP SYNDROME
Definition and Epidemiology (BMC Pregnancy Childbirth 2009;9:8)
• Variant of sev preeclampsia characterized by microangiopathic hemolysis, elevated serum transaminases, & low platelet count. Partial HELLP includes those w/ sev preeclampsia & those w/ either “ELLP” (elevated liver transaminase & low Plts) or “EL” (elevated liver enzymes). “Partial HELLP” = “sev preeclampsia,” on a spectrum. See also Chapters 11 and 12.
• 0.5–0.9% of all pregnancies. 10–20% of those w/ eclampsia. See Chapter 18.
• Increased risk for eclampsia, preterm birth, & perinatal mortality
Pathophysiology
• Microangiopathic hemolysis leading to elevation of serum lactate dehydrogenase level & fragmented red bld cells on periph smear. Same process as PEC, but more severe.
• Decreased Plts due to increased consump.
Clinical Manifestations
• Signs & sx of preeclampsia (elevated BP, proteinuria, focal edema, HA, vision changes)
• RUQ abdominal or midepigastric pain, nausea, vomiting
• Intensity of sx characterized by exacerbation during the night & recovery during day (J Matern Fetal Neonatal Med 2006;19:93)
• Sev complications: Spont rupture of subcapsular liver hematoma, placental abruption, DIC
Physical Exam and Diagnostic Workup/Studies (Am J Obstet Gynecol 2011;205:192)
• RUQ or epigastric tenderness
• Differing diagnostic criteria reported, 2 most common:
Sibai criteria: Hemolysis on periph smear, LDH > 600 U/L, or total bilirubin >1.2 mg/dL
+ AST > 70 U/L
+ Thrombocytopenia < 100000 cells/mm3
Martin criteria: LDH > 600 U/L
+ AST or ALT > 40 IU/L
+ Platelet count < 150000 cells/mm3
• Abdominal imaging (RUQ US, CT, MRI) to assess hepatic hemorrhage that may result in subcapsular hematoma ± rupture. Consider if ↑↑ elevation in transaminases.
Treatment and Medications
• Rx similar as that for sev preeclampsia (eg, antihypertensives, magnesium sulfate, deliv after steroids [for FLM] if <34 w or earlier depending on severity of dz)
• Presence of HELLP → immediate deliv due to ↑ mat death (1%) & increased mat morbidities: Bld xfusion (25%), DIC (15%), wound disruption (14%), placental abruption (9%), pulm edema (8%), renal failure (3%), & intracranial hemorrhage (1.5%) (Obstet Gynecol 2004;103:983)
• Dexamethasone may improve sev thrombocytopenia, but probably does not improve outcomes (Cochrane Database Syst Rev 2010;(9):CD008148)
• Increased risk for recurrence of HELLP in subseq pregnancies (5–25%); higher incid of preterm deliv, fetal-growth restriction, placental abruption & cesarean deliv in subseq deliveries w/o recurrence of HELLP
ACUTE FATTY LIVER OF PREGNANCY (AFLP)
Definitions and Epidemiology
• Accum of microvesicular fat a/w Mitoc dysfxn & impairment of hepatocyte fxn that can result in acute liver failure
• 1/10000 pregnancies
• A/w Mitoc abnormalities of fatty acid oxidation from autosomal inherited mut (ie, LCHAD deficiency)
• Occurs more often w/ nulliparas, male fetus, preeclampsia, & multifetal gest
Clinical Manifestations
• Presents late in 3rd trimester – often w/ PTL or lack of fetal mvmt
• Nonspecific sx including persistent nausea & vomiting, malaise, fatigue, anorexia, epigastric pain, progressive jaundice, low-grade fever
• 50% w/ sx concerning for preeclampsia including HTN, proteinuria, edema
• If sev: Ascites, coagulopathy & spont bleeding, SOB due to pulm edema, stillbirth, hepatorenal syn, hepatic encephalopathy, renal failure
Diagnostic Workup/Studies
• Labs: LFTs – ↑ bilirubin (>10 mg/dL), ↑ AST/ALT (typically less than 1000 U/L), CBC (hemoconcentration, leukocytosis, thrombocytopenia), coags (hypofibrinogenemia, hypoalbuminemia, hypocholesterolemia, prolonged clotting times, prolonged PT), hypoglycemia, or hyperglycemia secondary to pancreatitis
• Mother should undergo testing for LCHAD; can be lifesaving for neonate/inform risk for future pregnancies
• Imaging – RUQ US shows increased echogenicity; CT &/or MRI demonstrates lower liver density
• Liver bx, std for confirming dx but rarely used in clinical practice, shows microvesicular steatosis
Treatment and Medications
• Supportive care: Gluc infusion, reverse coagulopathy, fluid resusc
• Deliv recommended when dx confirmed; spont resolution after deliv, typically takes 1-w postpartum for hepatic dysfxn to resolve. During recovery period, 25% w/ transient diabetes insipidus & 50% w/ acute pancreatitis.
• May recur in subseq pregnancies, even if no LCHAD mut in mother. Historically w/ 70% mat mortality rate, improved w/ early dx to <10%.
• Perinatal mortality 13% due to high rate of preterm deliv
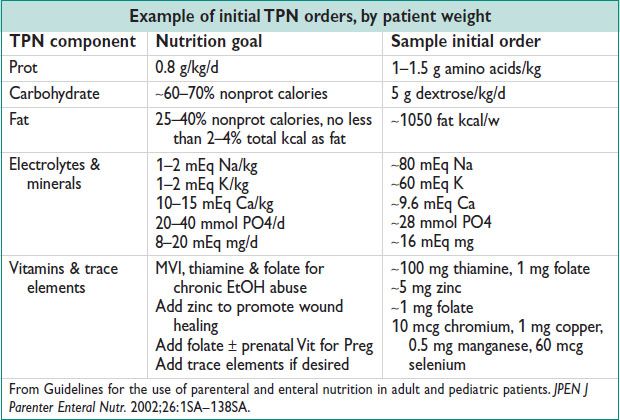
TOTAL PARENTERAL NUTRITION (TPN)
Definition, Indications, and Contraindications
• TPN: Intravenous supplementary nutrition including prot, caloric fat & dextrose, electrolytes, vitamins, minerals, & fluids. Generally a temporary intervention for severely limited po intake (eg, intractable vomiting/diarrhea, gastrointestinal ischemia, high output fistula) or conditions of sev bowel dysfxn (eg, bowel obst, protracted ileus).
• Contraindications: Hyperosmolality, sev hyperglycemia, sev electrolyte abnormalities, vol overload, sepsis. Not recommended in advanced cancer (J Parenter Enteral Nutr 2009;33(5):472).
Ordering TPN
• Parameters depend on specific dysfxn; consult nutritionist for TPN regimen
• TPN initiated w/ slow continuous feed, can be advanced to 12-h cycle if tolerated
TPN Monitoring
• Baseline: Chemistry panel, LFTs, lipids, albumin, transferrin, prealbumin
• Daily (while increasing feed rates): Electrolytes, fluid balance, gluc ≥4×/d
• Weekly: Triglycerides, LFTs, albumin, transferring, prealbumin
• Insulin sliding scale initially & transition to insulin in TPN mix when feasible
Complications
• Access related: Line infxn, PTX, hemothorax, brachial plexus injury; metabolic effects: Hyperglycemia, electrolyte alterations (ie, hyperK), nutrient excess or deficiency, Wernicke encephalopathy, hepatic dysfxn, refeeding syn (hypophos, hypokalemia, hypomagnesemia)
• Fetal complications of mat TPN uncommon; supplement Vit K for pregnant patients on TPN, & follow serial growth sonos (Obstet Gynecol 2003;101(5 Pt 2):1142)
< div class='tao-gold-member'>



