98 Fungal Infections
Candida Albicans
Clinical Manifestations and Management
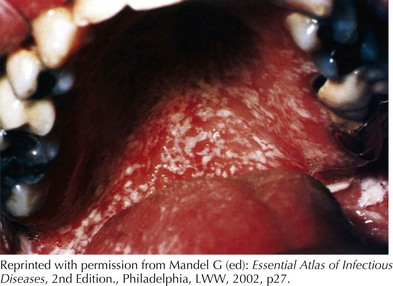
Oral candidiasis, also known as oral thrush, is a candidal infection of the oral-pharyngeal mucosa (Figure 98-1). It can affect up to 2% to 5% of otherwise healthy newborn infants and present as early as 7 to 10 days of life. In immunocompetent children, it is most common in infants and presents as adherent white plaques on the buccal or gingival mucosa. Removal of these plaques can result in localized bleeding. It can present with no symptoms or with increased fussiness and decreased feeding. Oral thrush is uncommon in children older than 12 months except after antibiotic use. Without recent antibiotic use, one may consider a primary immunodeficiency, diabetes mellitus, or HIV infection. Pseudomembranous candidiasis can be diagnosed clinically or by the identification of yeast cells and pseudohyphae by Gram stain or potassium hydroxide prep. Thrush can be treated with nystatin applied directly to the oral mucosa for 7 to 10 days. Thrush caused by antibiotic use generally resolves as the offending agent is discontinued. Bottle nipples and pacifiers should be sterilized as well to prevent reinfection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree