CHAPTER 56 Frequency, urgency and the painful bladder
Introduction
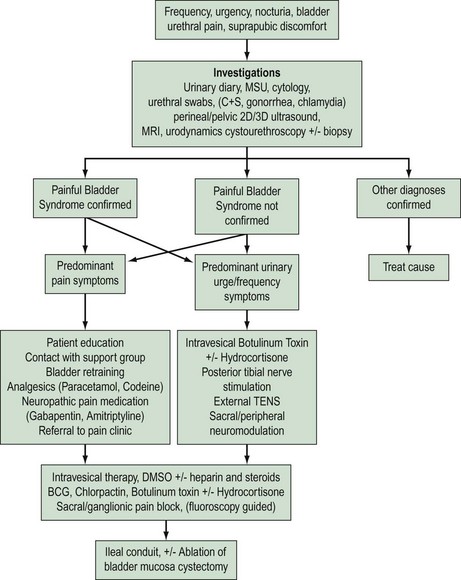
‘Cystitis’ is a term used for irritative urinary symptoms of frequency, urgency, suprapubic pain and dysuria. These symptoms of altered lower urinary tract sensation may be of recent onset (acute), longstanding (chronic) or recurrent. They may be caused by a variety of intravesical pathology such as infection, calculi, drug-induced inflammation, non-infective inflammatory processes due to local [e.g. painful bladder syndrome (PBS)] or systemic conditions (e.g. sarcoidosis), benign or malignant lower urinary tract tumours, or extravesical pelvic pathology such as pelvic masses (e.g. fibroids, endometriosis). Accurate diagnosis, appropriate intervention and therapy requires careful patient evaluation and a sound understanding of the differential causes (Figure 56.1).
Definitions
The Standardisation Sub-committee of the International Continence Society (ICS) published a terminology statement on lower urinary tract function in 2002 (Abrams et al 2002a,b). The majority of the following definitions are based on this statement.
24-h frequency is the total number of daytime voids and episodes of nocturia during a 24-h period.
Haematuria is an important symptom that requires urgent evaluation to exclude carcinoma.
Prevalence
A population-based study on the prevalence of lower urinary tract symptoms showed that the most commonly reported storage symptom in women is nocturia (54.5%). Urgency occurs in 12.8% and frequency in 7.4% of women. If nocturia is defined as two or more nocturnal micturitions per night, instead of one or more, the prevalence is decreased to 24% (Irwin et al 2006). PBS is a common condition in women, with reported prevalence of 1.7% in those aged under 65 years and 4% in those aged over 80 years. The vast majority of women with PBS have moderate or severe symptoms (Lifford and Curhan 2009).
Aetiology
Irritative bladder symptoms can be caused by a number of conditions originating within the lower urinary tract (Box 56.1). Infection and functional disorders, such as detrusor overactivity or voiding dysfunction, may cause urge symptoms and should be excluded. These conditions should be differentiated from more generalized systemic disorders (e.g. pregnancy, diabetes mellitus, renal disease), pelvic inflammatory disease or gynaecological surgery. A pelvic mass may cause urge-frequency symptoms due to bladder compression.
Box 56.1 Non-infective sensory disorders of the lower urinary tract
The aetiology of PBS is poorly understood. Several theories have been proposed over the years, including infection, immunological factors, leaky urothelium due to glycosaminoglycan deficiency, mast cell activation and altered neural function. Consensus is developing regarding epithelial dysfunction, mast cell activation and neurogenic inflammation; all part of a possible inflammatory response (Elgavish 2009).
Assessment
Investigations
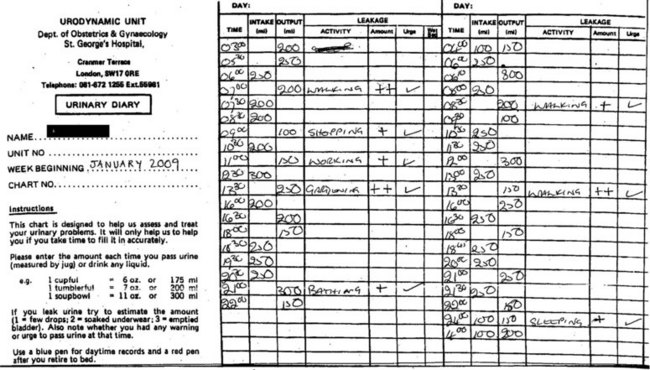
Urinary diary
A detailed 3-day urinary frequency–volume diary is an important part of the initial and ongoing assessment (Figure 56.2). These diaries are more accurate than patient recall, allowing rapid and accurate diagnosis of urinary frequency, nocturia, estimation of voided volumes, functional bladder capacity, and assessment of episodes of urgency, pain and incontinence as well as their temporal relationship. A diary will also educate the patient regarding voiding habits, and is essential for bladder retraining.
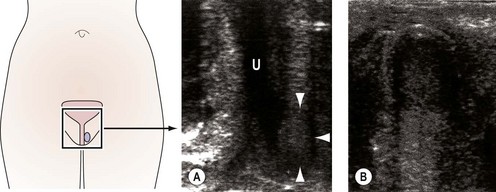
Imaging
Imaging of the urinary tract can be performed using ultrasound or contrast radiography, either alone or synchronously with urodynamic assessment [videocystourethrography (VCU)]. VCU demonstrates voiding function and can identify urethral obstruction, a urethral diverticulum or external compression due to fibroids or prolapse. Haematuria in the absence of identifiable uropathogens, negative cystoscopy or recurrent UTI is an indication for assessment of the upper urinary tract using contrast intravenous urography or urinary tract ultrasound. Ultrasound can also determine bladder residual volume and bladder wall thickness, and identify any structural abnormalities, including urethral diverticulae (Figure 56.3) (Doumouchtsis et al 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree