Chapter 4. Fluid and electrolytes
This chapter covers the common problems of fluid balance and management of infants with electrolyte disturbances that are faced on a daily basis. Other topics covered in this chapter are problems with glucose metabolism and inborn errors of metabolism.
QUESTION 1
The following maternal drugs cause acute renal failure in a baby (answer true or false):
i) Ibuprofen
ii) Aspirin
iii) Losartan
iv) Celecoxib
v) Gentamicin
vi) Captopril.
QUESTION 2
A baby born at 24 weeks gestation is being nursed on a platform with an overhead radiant heater. His birth weight is 600 g and he is receiving a total fluid of 1.5 mL/h. He is now 24 hours old and his blood results are as follows:
| Na | 149 mmol/L |
| K | 4.5 mmol/L |
| Urea | 9.4 mmol/L |
| Creat | 91 μmol/L |
| SBR | 85 μmol/L |
| CRP | 10 mg/L |
His urine output has been 3.5 mL since birth.
i) What is the most likely cause for this result?
a. Postnatal diuresis
b. Inappropriate ADH secretion
c. Inadequate water intake
d. Excessive water losses
e. Acute renal failure
f. Sepsis.
ii) What action would you take to improve the situation? Give two answers.
The next day, his blood results are as follows:
| Na | 145 mmol/L |
| K | 3.7 mmol/L |
| Urea | 8.4 mmol/L |
| Creat | 80 μmol/L |
| SBR | 160 μmol/L |
At this point the baby is on 120 mL/kg/day of 10% dextrose. His urine output has been 8 mL over the last 24 hours.
iii) Which of the following actions do you take next? Choose one answer.
a. Restrict fluid intake
b. Increase fluid intake to 150 mL/kg/day
c. Add additional sodium
d. Challenge with fluid bolus and diuretics
e. Observe and repeat U+E in 12 hours.
The next day his fluids are increased to 180 mL/kg/day. A loud systolic murmur becomes audible and pulses are bounding. Echocardiography shows evidence of a large ductus.
Urine output has been 18 mL over the last 24 hours. The following electrolytes are obtained:
| Na | 139 mmol/L |
| K | 3.9 mmol/L |
| Urea | 6.4 mmol/L |
| Creat | 70 μmol/L |
iv)
a. What changes would you make to his fluid regime?
b. Would you add sodium and potassium to his fluids?
Over the next 24 hours the baby’s respiratory condition deteriorates. A chest x-ray suggests moderate enlargement of the heart and a degree of pulmonary oedema. It is felt that the PDA is contributing significantly and the decision is made to commence indomethacin 0.6 mg/kg for 3 days. 24 hours later, the baby is thought to be more oedematous and the urine output has fallen to 0.4 mL/kg/hour with the following electrolytes:
| Na | 130 mmol/L |
| K | 4.2 mmol/L |
| Urea | 8.1 mmol/L |
| Creat | 92 μmol/L |
v) What do you think the most likely cause is for the current results?
vi) What action would you take?
vii) Which of the following measures of renal function could be helpful in distinguishing between prerenal and ischaemic acute renal failure?
a. Sodium
b. Potassium
c. Urea
d. Creatinine
e. Urine output
f. Urine osmolality
g. Urine microscopy
h. Urine sodium
i. Fractional excretion of sodium.
viii) At the age of 72 hours, you notice that his urine output is now 2.7 mL/kg/hour and his ventilation has significantly improved. Why is this?
QUESTION 3
You are asked to review a baby on the postnatal wards who is now 3 days old. Mum has had a caesarean section for failure to progress and is breast feeding the baby. The midwives are concerned that the baby is jaundiced. Birth weight 3.6 kg. On examination the baby is obviously jaundiced and is quiet.
i) What investigations/observations would you request?
The midwife has performed a test feed and thinks that a reasonable feed intake was achieved. She has weighed the baby before and after the feed.
ii) Does this help?
The investigations from a capillary blood sample reveal:
| Na | 157 mmol/L |
| K | 5.6 mmol/L |
| Urea | 12.8 mmol/L |
| Creat | 95 μmol/L |
| SBR | 286 μmol/L (unconjugated 6) |
| CRP | 8 mg/L |
| WBC | 11.6×10 9 (neutrophils 9.1) |
| Platelets | 242×10 9 |
| Hb | 21.5×10 9 |
| Film | normal |
| HCT | 68% |
| Weight | 2.9 kg |
iii) What is your first action?
Venous sample has comparable results with an HCT of 68%.
iv) What is the most important immediate action? Choose one answer.
a. Dilutional exchange transfusion
b. Glucose and insulin
c. ECG monitoring
d. Lumbar puncture
e. Intravenous fluids
f. NG feed.
v) How would you treat the baby? Which fluids would you consider using in immediate rehydration?
a. 10% dextrose
b. 5% dextrose
c. 0.9% saline
d. 0.45% saline
e. 0.18% saline / 5% dextrose.
vi) What complications can occur if this is not treated? List four.
QUESTION 4
You are called to see a baby on transitional care who was born at 36 weeks gestation, weighing 1.8 kg.The baby is now 4 hours old and had a bottle feed of 40 mL of formula milk an hour ago. The blood glucose is 1.8 mmol/L.
i) What action would you take?
a. Do nothing and reassure mum
b. Give another bottle feed and repeat blood glucose measurement
c. Carry out true laboratory glucose
d. Carry out full hypoglycaemia screen
e. Give bolus of intravenous dextrose
f. Give intramuscular glucagon.
Another bottle feed is offered and the infant takes a further 30 mL. A repeat blood glucose an hour later is 1.4 mmol/L.
ii) What action would you take?
You are unable to establish an intravenous infusion. The infant starts to vomit and repeat blood glucose is 0.8 mmol/L.
The baby is admitted to the neonatal unit and an infusion of 12.5% dextrose at 120 mL/kg/day is required to maintain the blood glucose above 2.6 mmol/L.
vi) What practical action should you take in regard to the baby’s high concentration of dextrose solution?
vii) Is this glucose infusion rate abnormally high?
viii) What is the most likely reason for this infant’s hypoglycaemia?
QUESTION 5
A term baby has suffered an asphyxial episode requiring full resuscitation at birth. Spontaneous respiration was not seen for 36 hours after birth although the heart rate had returned within 8 minutes of resuscitation.
A markedly abnormal CFAM was recorded and fits were treated with phenobarbitone, phenytoin and a midazolam infusion. The baby is now semi-comatose and breathing spontaneously and fitting has stopped. The baby has both a UVC and a UAC in situ.
Initial fluid replacement was 40 mL/kg/day of 10% dextrose with no additives and has been increased on day 3 to 90 mL/kg/day. Routine U+E analysis gives the following results.
| Na | 124 mmol/L |
| K | 3.6 mmol/L |
| Urea | 4.1 mmol/L |
| Creat | 35 μmol/L |
i) What explanation may account for this result? Choose the best answer.
a. Acute renal failure
b. Iatrogenic fluid overload
c. SIADH
d. Diabetes insipidus
e. Iatrogenic electrolyte depletion
f. Abnormal maternal electrolytes.
ii) What in the history supports your favoured diagnosis?
iv) Which of the following investigations would be most helpful? Choose two.
a. Urinary sodium
b. Urinary osmolality
c. Fractional excretion of sodium
d. Serial plasma sodium
e. Renin-angiotensin-aldosterone measurements
f. Renal ultrasound
g. Serum ADH levels
h. Plasma osmolality.
QUESTION 6
A 2-day-old term baby has a total plasma calcium of 1.7 mmol/L; ionised calcium is 0.65 mmol/L. The baby is well.
i) Which of the following is the most likely? Choose one answer.
a. Normal phenomenon
b. Pseudohyperparathyroidism
c. Infant of diabetic mother
d. Maternal elevated vitamin D intake
e. Exchange transfusion
f. Diuretic therapy
g. Hypoalbuminaemia
h. Maternal hypoparathyroidism
i. Low calcium intake
j. Perinatal asphyxia
k. PTH resistance
l. Hypoparathyroidism
m. IUGR
n. Maternal anticonvulsants
o. Maternal anti-TB therapy.
ii) Explain why you feel the other diagnoses are less likely.
iii) How do you treat the baby?
QUESTION 7
A preterm infant born at 28 weeks received one week of diuretic therapy following diagnosis of a PDA. The clinical course thereafter was uneventful. A renal ultrasound performed at 36 weeks corrected gestational age (as part of the screen for suspected UTI) revealed bilateral nephrocalcinosis.
The parents want to know how this has happened and what the long-term consequences are for their baby. What will you tell them?
QUESTION 8
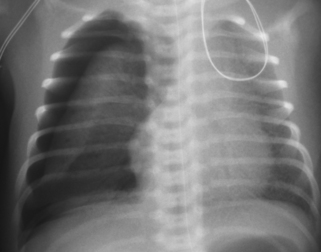
A term baby is born following a severe antepartum haemorrhage and requires full resuscitation. A diagnosis of hypoxic–ischaemic encephalopathy is made. At 48 hours the baby is still ventilated because of a lack of respiratory effort. The following ECG is obtained.
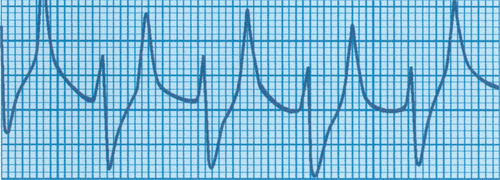 |
| Figure 4.1. |
i) What does this show?
ii) What is the underlying cause?
iii) What is the treatment? Give six key elements.
QUESTION 9
A baby suddenly collapses on the postnatal ward at the age of 36 hours. Prior to collapse, his feeding had deteriorated and he had started to vomit. On examination the baby is lethargic and tachypnoeic. Examination is unremarkable.
i) What is your differential diagnosis? Give four possibilities.
You bring the baby round to the neonatal unit and commence intravenous fluids and start antibiotics. Basic investigations are performed and results are as follows:
| CXR | Normal |
| Hb | 17.4g/dL |
| WCC | 9.4×10 9/L |
| Plat | 351×10 9/L |
| CRP | 11.3 mg/L |
| Blood glucose | 3.2 mmol/L |
The baby deteriorates and becomes more lethargic and drowsy.
ii) What urgent investigations would you now consider? Give four.
While awaiting the results of these investigations the baby becomes more tachypnoeic with marked recession. There is a sudden dramatic deterioration. Oxygen saturations fall to <40% and heart rate to <30.
iii) What differential diagnoses do you consider?
iv) What does it show and what would you do?
While dealing with this problem the results of your other investigations return; the results obtained are as follows:
| Echocardiogram | Normal |
| Ammonia | 350 μmol/L |
| Lactate | 3.4 mmol/L |
| Capillary blood gas | pH 7.48 |
| PCO 2 | 2.1 kPa |
| PO 2 | 3.2 kPa |
| BE | −8.0 mmol/L |
| Bic | 15.5 mEq/L |
v) What is the most likely diagnosis? Choose one answer.
a. Sepsis
b. Transient hyperammonaemia of the newborn
c. Organic acid defect
d. Fatty acid oxidation defect
e. Urea cycle defect
f. Congenital heart disease.
vi) What would be the basis of your management? Explain your decisions.
vii) What would you say to the parents?
QUESTION 10
A baby is found to have an anion gap of 27 mmol/L with an acidosis. Which two of the following are likely causes?




a. Propionic acidaemia
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree