Chapter 9 Fetal Surveillance during Labor
 Methods of Monitoring Fetal Heart Rate
Methods of Monitoring Fetal Heart Rate
CONTINUOUS ELECTRONIC FETAL MONITORING
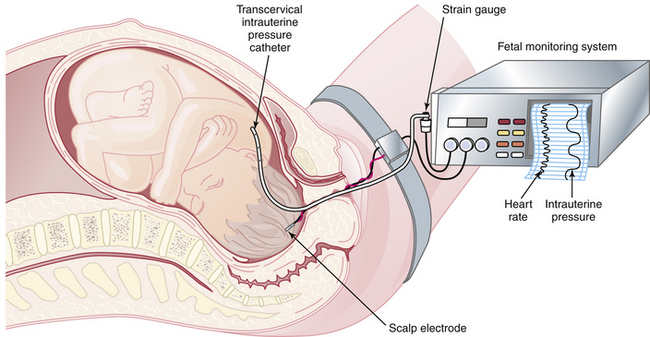
EFM allows continuous reporting of the FHR and uterine contractions (FHR-UC) by means of a monitor that prints results on a two-channel strip chart recorder. Uterine contractions result in a reduction in blood flow to the placenta, which can cause decreased fetal oxygenation and corresponding alterations in the FHR. The FHR-UC record can be obtained using external transducers that are placed on the maternal abdomen. This technique is used in early labor. Internal monitoring is carried out by placing a spiral electrode onto the fetal scalp to monitor heart rate and placing a plastic catheter transcervically into the amniotic cavity to monitor uterine contractions (Figure 9-1). To carry out this technique, the fetal membranes must be ruptured, and the cervix must be dilated to at least 2 cm.
 Etiology of Hypoxia, Acidosis, and Fetal Heart Rate Changes
Etiology of Hypoxia, Acidosis, and Fetal Heart Rate Changes
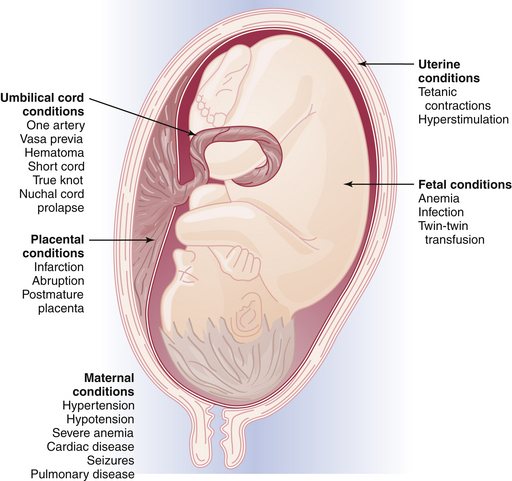
Fetal oxygenation can be impaired at different anatomic locations within the uteroplacental-fetal circulatory loop. For example, impairment of oxygen transportation to the intervillous space may occur as a result of maternal hypertension or anemia; oxygen diffusion may be impaired in the placenta because of infarction or abruption; or the oxygen content in the fetal blood may be impaired because of hemolytic anemia in Rh-isoimmunization. Figure 9-2 summarizes the clinical conditions that may be associated with fetal distress during labor.
FETAL HEART RATE PATTERNS
Baseline Assessment
This requires determination of the rate (in beats per minute) and the variability. Normal and abnormal rates are listed in Table 9-1. Baseline variability can be divided into short-term and long-term intervals. These are described as follows:
TABLE 9-1 BASELINE FETAL HEART RATES
| Rate | Beats/Minute |
|---|---|
| Normal | 120-160 |
| Abnormal | |
| Tachycardia | >160 |
| Bradycardia | <120 |
Types of Patterns
EARLY DECELERATION (HEAD COMPRESSION)
This pattern usually has an onset, maximum fall, and recovery that are coincident with the onset, peak, and end of the uterine contraction (Figure 9-3). The nadir of the FHR coincides with the peak of the contraction. This pattern is seen when engagement of the fetal head has occurred. Early decelerations are not thought to be associated with fetal distress. The pressure on the fetal head leads to increased intracranial pressure that elicits a vagal response similar to the Valsalva maneuver in the adult. The vagal reflex can be abolished by the administration of atropine, but this approach is not used clinically.