6
Fetal medicine
Chapter map
Multidisciplinary collaboration is the key to fetal medicine. Good contraceptive advice is important for the young person, while assisted conception allows more couples the joy of parenthood. Primarily an obstetric specialty, advice to the expectant couple often provides diagnostic and ethical problems, demanding input from paediatrics, genetics and surgery. You should understand that ultrasound, amniocentesis, chorionic villus sampling, fetal blood sampling, DNA analysis and fetoscopy allow assessment of fetal health, early detection of many anomalies and sometimes treatment of the fetus, taking Down syndrome and spina bifida as important examples.
6.2 Antenatal and pre-pregnancy care
6.3.1 Prenatal diagnosis (Table 6.2)
6.4 Embryonic and fetal growth and development
6.1 Control of fertility
6.1.1 Contraception
In developing countries, high birth rates and high child mortality tend to go hand in hand. Medical care reduces mortality from disease, but large family size threatens good nutrition, education, and socioeconomic growth. Safe, effective, cheap contraception coupled with education is key.
In Europe, the challenge of providing good, supportive advice to teenagers is widely acknowledged. The UK is now seeing a fall in the teenage pregnancy rate (around 40/1000 15–17 year olds), although it remains high compared with the rest of Europe.
 PRACTICE POINT
PRACTICE POINT6.1.2 Infertility treatment
Methods of helping infertile couples continue to advance. Techniques of ovulation control, in vitro fertilization, prolonged storage of gametes and the embryo, and surrogacy permit the separation of functions previously regarded as inseparable:
- Production of ova and sperm
- Place of fertilization
- The uterus in which the fetus develops
- The adult(s) responsible for rearing the child.
The ovum could come from Ms A, be fertilized in the laboratory by sperm from Mr B, be implanted in the uterus of Ms C and be reared by Mr and Ms D. This may raise psychosocial and ethical issues. Limiting the number of embryos implanted has reduced multiple pregnancies. Some studies raise concern that congenital abnormality may be more common after induced pregnancy.
6.2 Antenatal and pre-pregnancy care
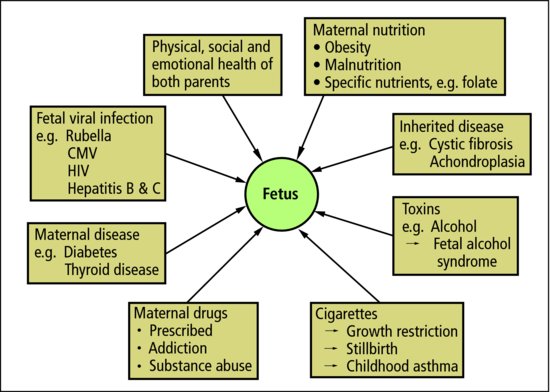
Preparation for a baby is aided by good physical and emotional health in both parents. Hereditary conditions should be discussed.
 PRACTICE POINT
PRACTICE POINTSome social and behavioural factors increase risk of problems:
- Socioeconomic deprivation: ↑ low birthweight; ↑ prematurity; ↑ perinatal mortality
- Young mothers: ↑ fetal growth problems; ↑ perinatal morbidity and mortality
- Older mothers: Down syndrome
- Obesity: ↑ gestational diabetes, ↑ perinatal mortality, ↑ difficult delivery
- Drug-abuse: effects of drugs on fetus and newborn
- Viral infection; HIV; hepatitis B and C.
Ideally, women should be in good health and prepared for pregnancy at the time of conception. The fetus may suffer long-term effects from early adverse influences (Figure 6.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree