The development of the fetus relies on the differentiation of primitive tissues into physiological systems, their complete development and their maturation. Thus, the differentiation of part of the mesoderm to form primitive lungs is established around week 5. The formation of lung structure is established between 24 and 28 weeks. The physiological maturation, requiring production by pneumocytes of surfactant, may occur later than this and is dependent in turn on maturation of the endocrine system.
Organ
Differentiation
Complete Formation
Spinal cord
3–4 weeks
20 weeks
Brain
3
28
Eyes
3
20–24
Olfactory apparatus
4–5
8
Auditory apparatus
3–4
24–28
Respiratory system
5
24–28
Heart
3
6
Gastro-intestinal system
3
24
Liver
3–4
12
Renal system
4–5
12
Genital system
5
7
Face
3–4
8
Limbs
4–5
8
Fetal Cardiovascular Development
CARDIOVASCULAR SYSTEM
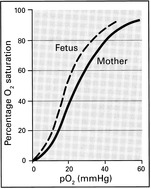
FETAL HAEMATOLOGY
FETAL LUNG DEVELOPMENT
MATERNAL PHYSIOLOGY
WEIGHT INCREASE
CARBOHYDRATE METABOLISM
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fetal and Maternal Physiology
The effect of drugs on fetal development is heavily dependent therefore on the gestation at the time of administration as well as the actual potential for teratogenicity of the agent concerned. This will be discussed later.
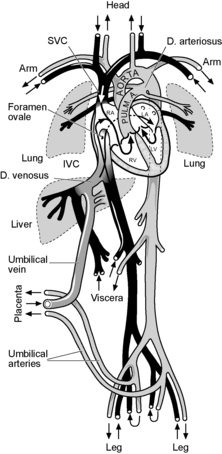
The respiratory function of the placenta requires that oxygenated blood be returned via the umbilical vein and into the fetal circulation. The changes which then occur at birth are dramatic.
Oxygenated blood from the placenta returns to the fetus via the umbilical vein. This vessel penetrates the liver and gives off small branches to that organ. Most of the blood is directed via the ductus venosus into the inferior vena cava which is carrying the returning non-oxygenated blood from the lower limbs, kidneys, liver, etc. There is only partial mixing of the two streams and most of the oxygenated blood is directed to the crista dividens at the upper end of the inferior vena cava through the foramen ovale into the left atrium and thence to the left ventricle and aorta.
The greatest volume of cardiac output from both ventricles, around 40%, goes to the placenta. The organ which receives the greatest flow is the brain which receives about 13%.
The autonomic nervous system is the principal control mechanism for fetal heart rate, stroke volume and blood pressure. In the first half of pregnancy control is chiefly by the sympathetic system. In the second half the parasympathetic system becomes increasingly dominant. It is this development which explains the reduction in fetal heart rate with advancing gestation.
The placenta is the organ of respiration for the fetus but adaptation to extra-uterine life requires that the lungs go through four recognised phases of development. The last of these, the terminal sac period, is when alveolar development occurs from 24 weeks gestation to term. Fetal breathing movements are established even before this and are required for proper anatomical development of the lungs. Absence of fetal breathing movements in later pregnancy may be a sign of fetal acidosis and its identification can be used to assess fetal well being. This will be discussed later.
During this time development of pneumocytes occurs and production of surface acting phospholipids is established. These components of surfactant are required to enable lung function to occur postnatally. Surfactant deficiency, a consequence of prematurity, causes respiratory distress syndrome in the newborn and is the greatest determinant of outcome in babies born preterm.
Nevertheless the alterations in the physiology require changes in energy consumption and use.
The energy demands of pregnancy derive from:
a) Basic physiological processes such as respiration, circulation, digestion, secretion, thermoregulation, growth and repair. These account for 66% of the total energy requirements in the non-pregnant female and amount to 1440 kcal/day. It is these processes which undergo greatest increase in pregnancy due to the demands of the fetus and placenta, uterus, breast growth, etc.
b) Activities of daily living. These account for 17% of the total energy use in the non-pregnant state, approximately 360 kcal/day. Advancing pregnancy usually entails some reduction in activity though there is great individual variation in this.
c) Work. The requirements associated with work differ with occupation but comprise around 10% for most women or 150–200kcal/day. This contribution to energy requirements generally reduces with advancing gestation, notably in the third trimester.
d) Specific dynamic action of food. Metabolism appears to be stimulated by food intake and comprises around 7% of the total or 150kcal/day. This should be met by increased consumption during pregnancy.
Overall there is a 14% increase in energy requirement during pregnancy.
During lactation a further increase is required for milk production and the total requirements will be in the region of 3000 kcal/day.
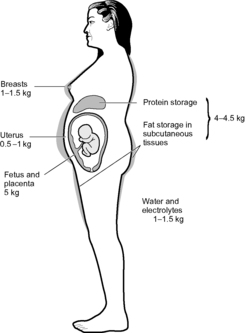
The increase is due to the growth of the conceptus, enlargement of maternal organs, maternal storage of fat and protein and increase in maternal blood volume and interstitial fluid.
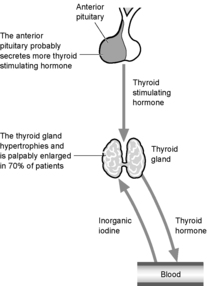
The increased metabolic rate is largely due to the fetus and leads to an increase in maternal oxygen consumption of around 20%. The factors governing this are chiefly endocrine. The pituitary gland enlarges and there is a 13% increase in size of the thyroid.
The fundamental hypothalamic–pituitary–thyroid relationships remain intact.
The blood sugar is maintained between 4.5 and 5.5mmol/litre (80–100mg/dl). Sugar which passes out in the renal glomerular filtrate is never in excess of the amount which can be reabsorbed by the tubules, and none appears in the urine.
A marked alteration in carbohydrate metabolism occurs in pregnancy.