Chapter 3 Female Reproductive Anatomy and Embryology
The scope of obstetrics and gynecology assumes a reasonable background in reproductive anatomy, embryology, physiology (see Chapter 4), and endocrinology (see Chapter 5 and Part 4). A physician cannot effectively practice obstetrics and gynecology without understanding the physiologic processes that transpire in a woman’s life as she passes through infancy, adolescence, reproductive maturity, and the climacteric. As the various clinical problems are addressed, it is important to consider those anatomic, developmental, and physiologic changes that normally take place at key points in a woman’s life cycle.
 Development of the External Genitalia
Development of the External Genitalia
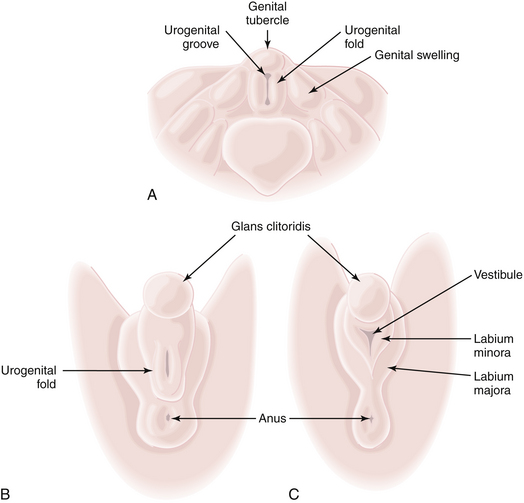
The external genitalia of the fetus are readily distinguishable as female at about 12 weeks (Figure 3-1). In the male, the urethral ostium is located conspicuously on the elongated phallus by this time and is smaller, owing to urogenital fold fusion dorsally, which produces a prominent raphe from the anus to the urethral ostium. In the female, the hymen is usually perforated by the time delivery occurs.
 Anatomy of the External Genitalia
Anatomy of the External Genitalia
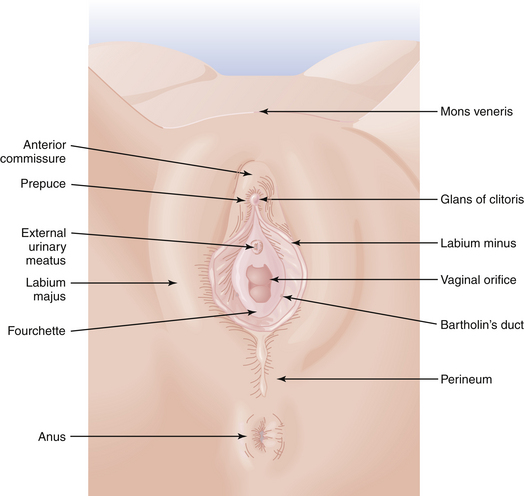
The perineum represents the inferior boundary of the pelvis. It is bounded superiorly by the levator ani muscles and inferiorly by the skin between the thighs (Figure 3-2). Anteriorly, the perineum extends to the symphysis pubis and the inferior borders of the pubic bones. Posteriorly, it is limited by the ischial tuberosities, the sacrotuberous ligaments, and the coccyx. The superficial and deep transverse perineal muscles cross the pelvic outlet between the two ischial tuberosities and come together at the perineal body. They divide the space into the urogenital triangle anteriorly and the anal triangle posteriorly.
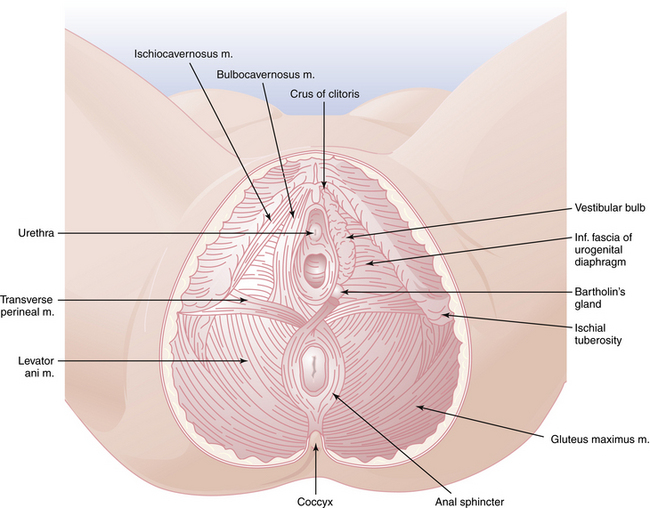
FIGURE 3-2 The perineum, showing superficial structures on the left and deeper structures on the right.
VULVA
The external genitalia are referred to collectively as the vulva. As shown in Figure 3-3, the vulva includes the mons veneris, labia majora, labia minora, clitoris, vulvovaginal (Bartholin’s) glands, fourchette, and perineum. The most prominent features of the vulva, the labia majora, are large, hair-covered folds of skin that contain sebaceous glands and subcutaneous fat and lie on either side of the introitus. The labia minora lie medially and contain no hair but have a rich supply of venous sinuses, sebaceous glands, and nerves. The labia minora may vary from scarcely noticeable structures to leaf-like flaps measuring up to 3 cm in length. Anteriorly, each splits into two folds. The posterior two folds attach to the inferior surface of the clitoris, at which point they unite to form the frenulum of the clitoris. The anterior folds are united in a hood-like configuration over the clitoris, forming the prepuce. Posteriorly, the labia minora may extend almost to the fourchette.
 Internal Genital Development
Internal Genital Development
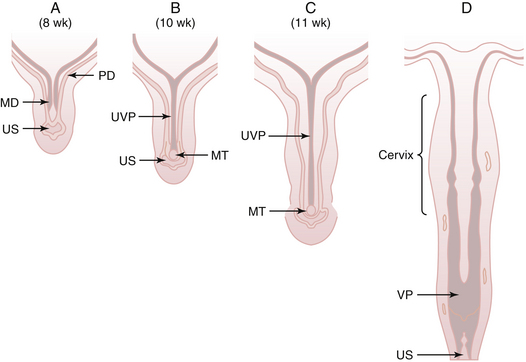
Mesonephric duct development occurs in each urogenital ridge between weeks 2 and 4 and is thought to influence the growth and development of the paramesonephric ducts. The mesonephric ducts terminate caudally by opening into the urogenital sinus. First evidence of each paramesonephric duct is seen at 6 weeks’ gestation as a groove in the coelomic epithelium of the paired urogenital ridges, lateral to the cranial pole of the mesonephric duct. Each paramesonephric duct opens into the coelomic cavity cranially at a point destined to become a tubal ostium. Coursing caudally at first, parallel to the developing mesonephric duct, the blind distal end of each paramesonephric duct eventually crosses dorsal to the mesonephric duct, and the two ducts approximate in the midline. The two paramesonephric ducts fuse terminally at the urogenital septum, forming the uterovaginal primordium. The distal point of fusion is known as the müllerian tubercle (Müller’s tubercle) and can be seen protruding into the urogenital sinus dorsally in embryos at 9 to 10 weeks’ gestation (Figure 3-4). Later dissolution of the septum between the fused paramesonephric ducts leads to the development of a single uterine fundus, cervix, and, according to some investigators, the upper vagina.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree