Chapter 26 Family Planning
REVERSIBLE CONTRACEPTION, STERILIZATION, AND ABORTION
When birth control methods in sexually active women are grouped into tiers based on their efficacy with typical use (Table 26-1), it becomes obvious that the most efficient methods are those that are long-term, convenient, and do not require any ongoing action from the woman (Tier 1). For example, the intrauterine devices (IUDs) and progestin implants provide the highest level of pregnancy protection, with first-year failure rates in typical use of less than 1% (Table 26-2). Other hormonal methods, such as the once-every-3-months injection, monthly vaginal rings, weekly patches, and daily pills are in tier 2. Each of these hormonal methods has the potential for very low pregnancy rates (1%), but in typical use, they have first-year failure rates of 7% to 8%. Tier 3 contraceptive methods are the barrier and behavioral methods. Here the differential between the potential that the method offers and what is really seen is widest. For example, male condoms have a less than 2% failure rate if used correctly and consistently with every episode of intercourse. However, in real life, the pregnancy rate is 17.4%. Female barrier methods (diaphragms, cervical caps, shields, and female condoms) have higher pregnancy rates. Interestingly, behavioral methods such as coitus interruptus and fertility awareness methods have rates that are almost equivalent to many barrier methods in typical use.
| Tier | Method of Contraception |
|---|---|
| 1: Longer term | Progestin implants and intrauterine devices |
| 2: Combined hormonal | |
| 3: Barrier and behavioral |
TABLE 26-2 CONTRACEPTIVE FAILURE RATES COMPARING TYPICAL USE AND PERFECT USE
| Contraceptive Method | Percent Failure within First Year of Use | |
|---|---|---|
| Perfect Use | Typical Use | |
| No method | 85 | 85 |
| Male sterilization | 0.10 | 0.15 |
| Female sterilization | 0.5 | 0.5 |
| Copper ParaGard T 380A IUD | 0.6 | 0.8 |
| Levonorgestrel-releasing IUD | 0.1 | 0.1 |
| DMPA | 0.3 | 6.7 |
| OC—combined | 0.3 | 8.7 |
| OC—progestin only | 0.5 | 8.7 |
| Diaphragm with spermicide | 6 | 16 |
| Condom—male, latex | 2 | 17.4 |
| Cervical cap—parous | 26 | 32 |
| Cervical cap—nulliparous | 9 | 16 |
| Spermicides | 15 | 29 |
| Fertility awareness | 19 | 25.3 |
| Withdrawal | — | 18.4 |
DMPA, depot medroxyprogesterone acetate; OC, oral contraceptive.
1. Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77(1):10–21
2. Hatcher RA, Trussell J, Nelson AL, Cates W Jr, Stewart FH, Kowal D. Contraceptive Technology, 19th ed. NewYork, Ardent Media, Inc. 2007.
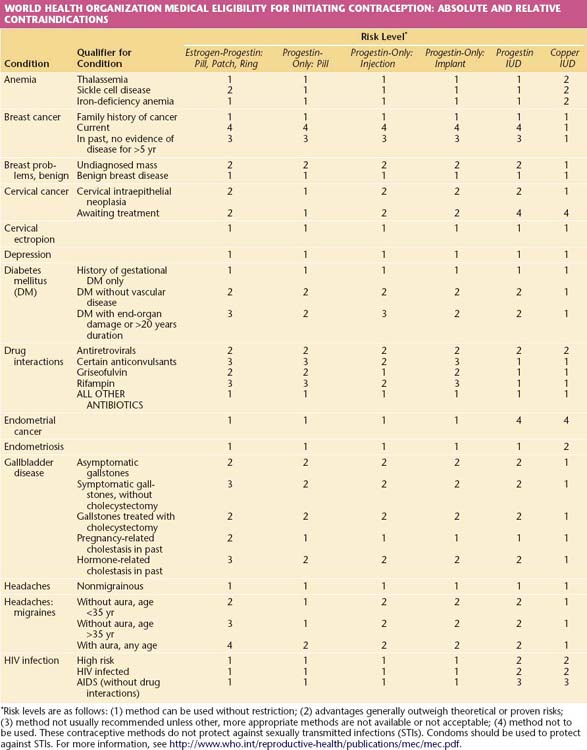
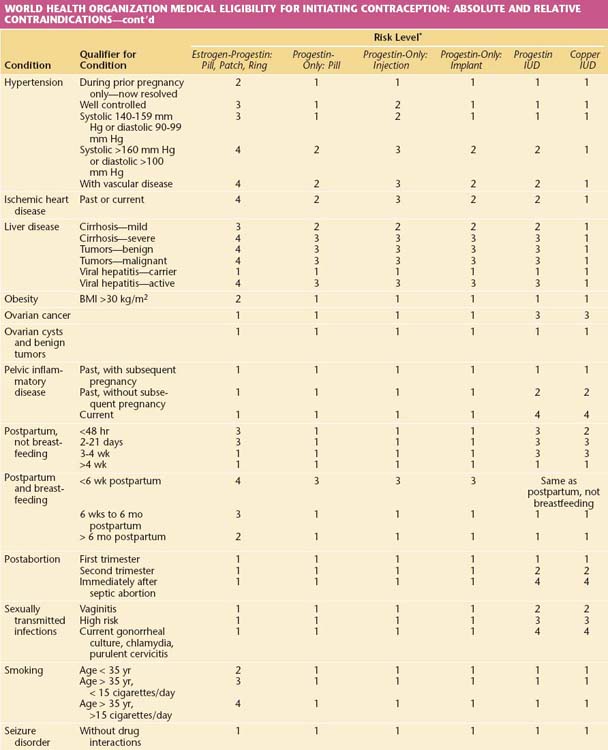
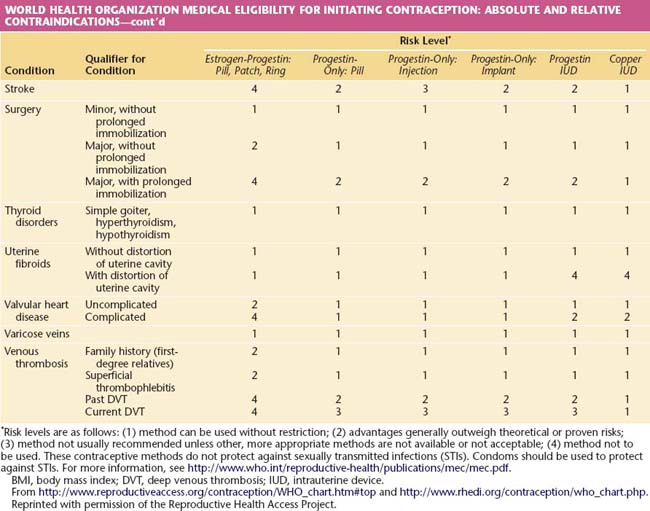
The safety of all methods of family planning is well established. In selecting options for an individual woman, the requirement is that any method offered must be safer to the woman’s health than pregnancy. It is from that perspective that the World Health Organization (WHO) has developed its Medical Eligibility Criteria (MEC; Table 26-3), which rates the appropriateness of each major contraceptive method in a variety of medical circumstances. Recommendations are made on a 1 to 4 scale, in which a rating of 1 indicates approval and 4 represents an absolute contraindication. This rating often differs from the labeling for individual products, which generally reflects theoretical concerns and desires by the manufacturers to protect themselves from product liability. Prescribers should act on evidence-based recommendations such as the WHO MEC.
TABLE 26-3 WORLD HEALTH ORGANIZATION MEDICAL ELIGIBILITY FOR INITIATING CONTRACEPTION: ABSOLUTE AND RELATIVE CONTRAINDICATIONS
 Contraception
Contraception
TIER 1 CONTRACEPTIVE OPTIONS
Intrauterine contraceptives and implants are the most effective, reversible methods available to women at risk for pregnancy. Typical failure rates closely correspond to those seen with correct use (see Table 26-2). Each is also very safe and can be used by women with serious medical conditions for whom pregnancy may be very dangerous.



