28 Eye Disorders
Ophthalmic diseases occur most often in the very young or elderly, with the exception of eye trauma, refractive errors, and some other disorders (e.g., retinoblastoma [RB]). Infants and children are particularly susceptible to permanent central visual loss (amblyopia), opacities (congenital cataracts), refractive errors not associated with amblyopia, strabismus (ocular misalignment), and other conditions that interfere with visual acuity (ptosis, anisometropia). With early detection and correction these conditions do not lead to permanent loss in the mature central visual system of the older child or adult (American Association for Pediatric Ophthalmology and Strabismus [AAPOS] and American Academy of Ophthalmology [AAO], 2007). When caring for children with eye problems, priorities include promoting optimal growth and development of the ocular structures and maximizing visual acuity. To this end, primary care providers (PCPs) seek to promote good vision and health, detect abnormalities, treat those conditions that fall within their scope of practice, refer patients with conditions requiring an ophthalmologist’s expertise, and provide education and reassurance to parents and children. Care of blind or visually impaired children is discussed in Chapter 15.
 Standards for Visual Screening and Care
Standards for Visual Screening and Care
• Increase the proportion of preschool children ages 5 years and younger who receive vision screening.
• Reduce blindness and visual impairment in children and adolescents ages 17 years and younger.
• Reduce uncorrected visual impairment due to refractive errors.
• Increase the use of personal protective eyewear in recreational activities and hazardous situations around the home.
• Screening tests have reasonable accuracy in identifying strabismus, amblyopia, and refractive errors in children younger than 5 years. Providers should be alert for signs of ocular misalignment when examining infants and children. Treating strabismus and amblyopia early greatly reduces long-term amblyopia and improves visual acuity.
• Well-child examinations should include ocular history, vision assessment, external inspection of the eyes (including pupils and red light reflex), lids, and ocular mobility. This also includes an evaluation of fixation and following (binocularly and monocularly) starting at birth, with patched visual acuity screening starting at 3 years old (Tables 28-1, 28-2, and 28-3). If the child is uncooperative, retesting should occur 6 months later. Inability to fix and follow after 3 months of age warrants a referral to a pediatric ophthalmologist or an eye specialist trained to treat pediatric patients. Subsequent testing should occur at 4, 5, 10, 12, 15, and 18 years old. A subjective historical assessment should occur during visits at all other ages. Children who are difficult to screen after two attempts or who demonstrate any other eye abnormality should undergo photoscreening techniques to detect amblyopia, media opacities, and treatable ocular disease processes.
TABLE 28-1 Normal Visual Developmental Milestones
| Birth-2 weeks | Infant sees and responds to change in illumination; refuses to reopen eyes after exposure to bright light; increasing alertness to objects; fixes on contrasts (e.g., black and white); jerky movements; pupillary reaction present. |
| 2-4 weeks | Infant fixes and follows on an object, though sporadically. |
| By 3-4 months | Infant recognizes parent’s smile; looks from near to far and focuses close again; beginning development of depth perception; follows 180-degree arc; reaches toward toy; few exodeviations; esotropia abnormal. |
| By 4 months | Color vision near that of an adult; tears are present. |
| By 6-10 months | Infant fixes on and follows toy in all directions; movements smooth. |
| By 12 months | Vision is close to fully developed. |
TABLE 28-2 Visual Acuity Norms (Snellen Equivalents)
| Forced Choice Preferential Looking (FPL) | Age Visual-Evoked Potential (VEP) | |
|---|---|---|
| Birth | 20/400 | 20/800 |
| 2 months | 20/400 | |
| 4 months | 20/200 | 20/600 |
| 6 months | 20/150 | 20/400 |
| 12 months | 20/50 | 20/20 |
| 18-24 months | 20/25 or 20/20 | |
| 5 years | 20/25 or 20/20 |
VEP does not require a motor response of the primary visual cortex. FPL may involve more cortical processing, which matures more slowly than the visual cortex.
Adapted from Eustis HS, Guthrie ME: Postnatal development. In Wright KW, Spiegel PH, editors: Pediatric ophthalmology and strabismus, New York, 2003, Springer; Stout A: Pediatric eye examination. In Wright KW, Spiegel PH, editors: Pediatric ophthalmology and strabismus, New York, 2003, Springer.
TABLE 28-3 Recommended Ages and Methods for Pediatric Eye Evaluation Screening
| Recommended Age | Method | Indications for Referral to an Ophthalmologist |
|---|---|---|
| Newborn-3 months | Red reflex | Abnormal or asymmetric |
| Ocular history | ||
| Inspection | Structural abnormality | |
| 3-6 months (approximately) | Fix and follow | Failure to fix and follow in a cooperative infant |
| Ocular history | ||
| Red reflex | Abnormal or asymmetric | |
| Inspection | Structural abnormality | |
| 6-12 months and until child is able to cooperate for verbal visual acuity | Fix and follow with each eye | Failure to fix and follow |
| Alternate occlusion | Failure to object equally to covering each eye | |
| Ocular history | ||
| Corneal light reflex | Asymmetric | |
| Red reflex | Abnormal or asymmetric | |
| Inspection | Structural abnormality | |
| ≥3 years and every 1-2 years after 5 years | Visual acuity* (monocular) | 3 years: 20/50 or worse; 5 years: 20/40 or worse |
| Ocular history | >5 years: 20/30 or worse, or two lines of difference between the eyes | |
| Corneal light reflex/cover-uncover reflex | Asymmetric/ocular refixation movements | |
| Red reflex | Abnormal or asymmetric | |
| Inspection | Structural abnormality | |
| Attempt ophthalmoscopy |
Note: These recommendations are based on panel consensus. Although the child may be retested if screening is inconclusive or unsatisfactory, undue delays should be avoided; if inconclusive on retesting, referral for comprehensive pediatric medical eye evaluation is indicated. Use of medication for pupillary dilation facilitates evaluation of the red reflex. See text for recommended medication.
* Pictures (Lea Hyvärinen [LH/LEA] symbols or Allen cards for 2- to 4-year-olds); “tumbling E” or HOTV for ≥4-year-olds; or vision-testing machines.
Data from American Academy of Pediatrics (AAP) Committee on Practice and Ambulatory Medicine and Section on Ophthalmology, American Association of Certified Orthoptists, American Association of Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology (AAO): Eye examination in infants, children, and young adults by pediatricians: policy statement, Pediatrics 111(4):902-907, 2003, reaffirmed 2007.
• Health and developmental problems that make screening by the primary care clinician difficult or inaccurate (e.g., retinopathy of prematurity [ROP], or diagnostic evaluation of a complex disease with ophthalmologic manifestations)
• A family history of conditions that cause or are associated with eye or vision problems (e.g., RB, significant hyperopia, strabismus [particularly accommodative esotropia], amblyopia, congenital cataract, or glaucoma)
• Multiple health problems, systemic disease, or the use of medications that are known to be associated with eye disease and vision abnormalities (e.g., neurodegenerative disease, juvenile rheumatoid arthritis, systemic steroid therapy, systemic syndromes with ocular manifestations, or developmental delay with visual system manifestations).
 Development, Physiology, and Pathophysiology of the Eye
Development, Physiology, and Pathophysiology of the Eye
Anatomy and Physiology of the Eye
The eyeball consists of three layers of tissue: the fibrous tunic, the vascular tunic, and the inner tunic or retina. The fibrous tunic consists of the sclera and the cornea. The vascular tunic, the middle layer, is composed of the choroid, the ciliary body, and the iris (Fig. 28-1). All the structures of the eye are dedicated to accurate and efficient functioning of the innermost layer of the eyeball, the retina. The optic disc consists only of nerve fibers (no rods or cones), so no visual images are formed here. Thus, it is referred to as the blind spot.
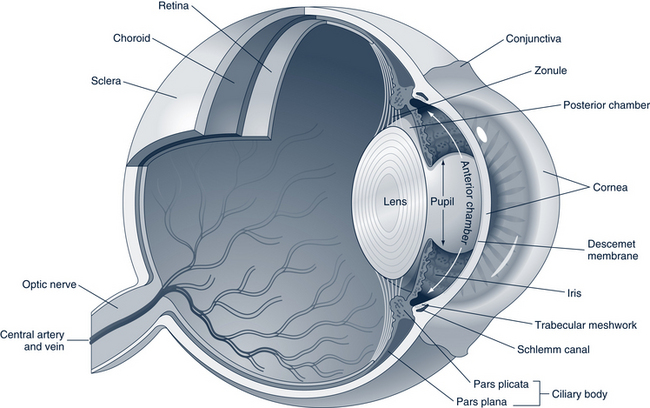
FIGURE 28-1 Anatomy of the eye.
(From Kumar V, Abbas AK, Fausto N, et al: Robbins and Cotran pathologic basis of disease, professional edition, ed 8, Philadelphia, 2010, Saunders.)
The inside of the eyeball consists of the anterior and posterior cavities (see Fig. 28-1). The anterior cavity is divided into anterior and posterior chambers. The anterior chamber lies between the cornea and the iris. The posterior chamber lies between the iris and the suspensory ligament. Aqueous humor circulates throughout these chambers to maintain intraocular pressure (IOP) and link the circulatory system with the avascular lens and cornea. The other cavity within the eyeball, the posterior cavity, lies between the lens and the retina. The gelatinous vitreous humor found in this cavity contributes to the maintenance of IOP and holds the retina in place. The lens, which separates the cavities, hangs by the suspensory ligament. Six muscles guide movement of the globe. Four rectus muscles (superior, inferior, lateral, and medial) move the eyeball up, down, in, and out, respectively. Two oblique muscles (superior and inferior) rotate the eyeball on its axis. Cranial nerve (CN) III (oculomotor), CN IV (trochlear), and CN VI (abducens) innervate these muscles.
The focusing of light rays involves four basic processes: refraction of light rays, accommodation of the lens, constriction of the pupil, and convergence of the eyes. Refraction is the bending of light rays as they pass from one transparent medium (air) to another (cornea or lens). The lens modifies the degree of refraction to create the sharpest image on the retina. Accommodation is the ability of the lens to focus on close objects by increasing its curvature. The normal eye refracts light rays from an object 20 feet away to focus a clear image onto the retina; hence the fraction 20/20 is used to denote the accepted standard of normal vision. The circular muscle fibers of the iris, which contract in response to light, cause constriction of the pupil. Regulating the light entering the eye can also facilitate production of a precise image. To maintain single binocular vision, close objects require the eyes to rotate medially so that the light rays from the object hit the same points on both retinas. This rotation is called convergence. A normal neonate demonstrates disconjugate fixation, but convergence and accommodation normally develop by 3 to 4 months, with parallel alignment by 5 to 6 months without nystagmus or strabismus. Jerky eye movements can be seen until 2 months, after which time smooth tracking movements are expected.
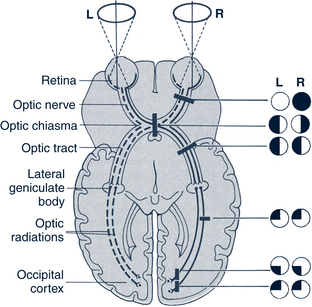
After an image is formed on the retina, light impulses are converted into nerve impulses and transmitted to the visual centers located in the occipital lobes of the cerebral cortex. Lesions in various places along the neural tracts from the eye to the cortex cause different types of loss of visual fields (Fig. 28-2).
 Assessment
Assessment
History
• General medical history including birthweight; pertinent prenatal, perinatal, postnatal factors (e.g., prematurity, infections); past hospitalizations and surgery; general health and development
• Family medical history of ocular problems (including eye surgeries), such as glaucoma, blindness, poor vision, difficulty walking in dim light, photophobia, use of thick glasses, lazy eye, strabismus, nystagmus, leukokoria, RB, congenital cataracts
• History of chronic systemic disease in patient or family (e.g., inflammatory bowel disease; connective tissue disorders; cardiac defects of Marfan syndrome; midfacial hypoplasia; abnormalities of teeth, umbilical cord, or urinary tract; neurologic or skin anomalies; developmental delay; mental retardation; diabetes; sickle cell hemoglobinopathies; Tay-Sachs disease; tuberculosis)
• Presence of allergies and specific allergens
• Current medications (e.g., steroids); past or present substance abuse
• Child’s ocular history, which includes:
 Date (and results) of the last vision screening and prior eye problems or diseases, including diagnoses and treatments
Date (and results) of the last vision screening and prior eye problems or diseases, including diagnoses and treatments If history of eye injury: unilateral or bilateral injury? Were there visual changes or photophobia? What treatment was received?
If history of eye injury: unilateral or bilateral injury? Were there visual changes or photophobia? What treatment was received? Prescription and use of eyeglasses or contact lenses. Does the child have glasses that were prescribed? Are they used? If not, why?; use of sunglasses with ultraviolet (UV) protection or protective eyewear for sports activities
Prescription and use of eyeglasses or contact lenses. Does the child have glasses that were prescribed? Are they used? If not, why?; use of sunglasses with ultraviolet (UV) protection or protective eyewear for sports activities• Symptoms or indications of eye dysfunction or disease:
 Older children may report visual loss or change in vision, such as blurring, diplopia, spots, and halos. Younger children may be observed to have problems with fixing or focusing (holding objects up close to see), tracking, squinting, head tilt, eye-hand coordination, grasp, gait, balance, behavior, and changes in the ability to maintain eye contact; eyelid droop
Older children may report visual loss or change in vision, such as blurring, diplopia, spots, and halos. Younger children may be observed to have problems with fixing or focusing (holding objects up close to see), tracking, squinting, head tilt, eye-hand coordination, grasp, gait, balance, behavior, and changes in the ability to maintain eye contact; eyelid droop Swollen eyelids, pruritus, excessive tearing or discharge, erythema, burning, eye fatigue, strabismus
Swollen eyelids, pruritus, excessive tearing or discharge, erythema, burning, eye fatigue, strabismusPhysical Examination
The physical examination can be challenging, depending on the child’s age. The components need to be done quickly to accommodate the child’s short attention span. Knowledge of visual developmental milestones is essential in assessing a child’s visual capabilities (see Table 28-1).
• Gross inspection should be made of the external structures with a penlight (lids, bulbar and palpebral conjunctiva, cornea, lacrimal structures, and the size, symmetry, and reactivity of the pupils), orbits, eye muscle balance, and mobility.
• The red reflex is tested in all ages. It needs to be assessed for color, intensity, and clarity (opacities or white spots). A rule of thumb is that if the examiner cannot see into the eye (e.g., absent red light reflex), the patient cannot see out.
• In children more than 5 years old, funduscopic examination allows for visualization of the retina, choroid, fovea, macula, optic disc and cup, and entry and exit of the vessels and nerves.
• Examination of the eye is sometimes facilitated by using a cotton-tipped applicator to evert the eyelid. Eyelid eversion is accomplished by having the patient look down while the examiner grasps the lashes with the thumb and index finger, places the applicator in the middle of the lid, pulls the eyelid down and out, and everts it over the applicator.
• Growth parameters (especially head growth and shape) and the head and neck or other structures should be examined if a systemic condition is suspected.
Screening Tests
Red Light Reflex
• Darken the examination room (a lighted room causes the pupils to constrict, resulting in a poor red reflex). The darker the room, the easier it is to detect more subtle asymmetries between the red reflexes.
• Stand an arm-length away from the infant or child and use the ophthalmoscope light set at 0 or +1 to illuminate the face.
• Look at both pupils simultaneously and separately. Examining the red reflex slightly off axis to the center of the pupil enhances the color (ask a child to look to one side or use a distraction; infants can be approached from the side). In children with fair skin pigmentation, the red reflex is bright red-orange; in those with darker pigmentation, the red reflex is dark red-brown.
• The red reflexes should be symmetric; any asymmetry, dark or white spots, opacities, or leukokoria (white pupillary reflex) requires either:
 Dilation of the pupils. Dilation may be used to enhance the examination in questionable situations. In infants younger than 9 months, use 0.25% cyclopentolate with 2.5% phenylephrine. In infants older than 9 months, use the cyclopentolate/phenylephrine drops or 1% tropicamide ophthalmic drops (AAP et al, 2008). One or 2 drops are instilled in each eye at least 15 minutes prior to the examination. Rare side effects to these medications include tachycardia, hypertension, urticaria, cardiac arrhythmias, or contact dermatitis.
Dilation of the pupils. Dilation may be used to enhance the examination in questionable situations. In infants younger than 9 months, use 0.25% cyclopentolate with 2.5% phenylephrine. In infants older than 9 months, use the cyclopentolate/phenylephrine drops or 1% tropicamide ophthalmic drops (AAP et al, 2008). One or 2 drops are instilled in each eye at least 15 minutes prior to the examination. Rare side effects to these medications include tachycardia, hypertension, urticaria, cardiac arrhythmias, or contact dermatitis.Visual Acuity Testing
Visual acuity screening (see Tables 28-2 and 28-3), for both near and distance vision, should be performed on all children during routine physical examinations, when problems with visual acuity are suspected, and/or when eye trauma occurs. The American Optometric Association recommends comprehensive examinations at 6 months, 2 and 4 years, and every 2 years afterward (AOA, 2002). The AAO recommends a formal screening by the age of 5 years and sees no added benefit in having comprehensive examinations for asymptomatic children (AAPOS and AAO, 2007). If the child wears eyeglasses or contact lenses, visual acuity measurement must be obtained with correction.
Testing for Ocular Mobility and Alignment
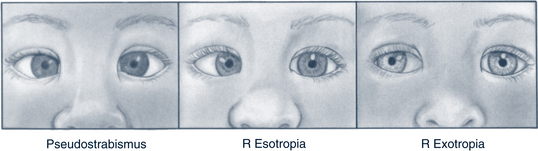
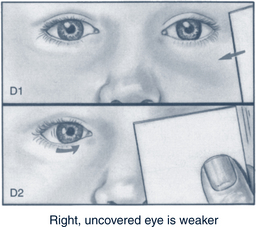
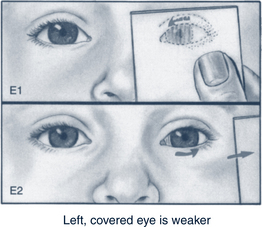
The Hirschberg test (also called the corneal light reflex) evaluates extraocular muscle function by projecting a small light source onto the cornea of the eye with the child looking straight ahead. A normal test reveals the reflected light as a small white dot symmetrically located in the same position of each eye (often slightly nasal of center). The cover-uncover test and the alternating cover test should be performed with the child fixating straight ahead, first on a near point object and then on a far point object about 20 feet away (Fig. 28-3). The process is sometimes aided by asking the child questions about the object (e.g., “How many cows do you see?” in a picture that has been placed for this purpose on the wall). During the alternating cover test, the examiner rapidly covers and uncovers the eye while shifting between the two eyes. Any orbital movement is an indication of misalignment.
Assessment of Visual Loss
• Shine a penlight into the eye from a lateral position and turn the light off and on several times to assess light perception. If the child can identify when the light is on or off, vision is described as “LP” (light perception).
• If hand movement (H/M) can be seen 12 inches from the child’s face, it is documented as “H/M at 1 ft.” Indication of search and recognition should be seen as the hand is slowly moved back and forth with periodic cessation.
• Ask the child to count the number of fingers (C/F) seen when one, two, or three fingers are held up 12 inches from the child’s face. If the child is correct, document the vision as “C/F at 1 ft.”
 Management Strategies
Management Strategies
Referral for Ophthalmologic and Specialty Management
See Table 28-4 for guidance on when to refer for a more comprehensive examination. Although any child with eye pathologic conditions should be referred to an ophthalmologist, optometrists can be a valuable resource in caring for children with refractive errors or certain common eye conditions (e.g., corneal abrasions, foreign bodies). PCPs should acquaint themselves with the statutory guidelines for scope of practice and prescription privileges as designated by the state boards of optometry within their state to optimize referral possibilities.
TABLE 28-4 Indications for a Comprehensive Pediatric Medical Eye Evaluation
Note: These recommendations are based on panel consensus.
* Headache is not included because it is rarely caused by eye problems in children. This complaint should first be evaluated by the primary care physician.
From American Academy of Ophthalmology (AAO) Pediatric Ophthalmology Panel: Pediatric eye evaluations: screening and comprehensive ophthalmic evaluation PPP, 2007. Available at www.one.aao.org/ce/practiceguidelines/ppp_content.aspx?cid=761ac199-5cfe-42f4-b40b-33f9d5f0d364 (accessed Nov 8, 2010).
Corrective lenses
General guidelines for glasses and contact lenses can be found in Box 28-1. Glasses must be changed frequently in children because of head growth. Because the child may be reluctant to wear eyeglasses that hurt or pinch, parents should assess the fit of the eyeglasses on a monthly basis and watch for behavior that indicates discomfort in a preverbal child (e.g., constantly removing glasses, rubbing at the frames or face).
BOX 28-1 Recommendations for Use of Corrective Lenses
Eyeglasses
• Polycarbonate lenses are lightweight, strong, and shatterproof; scratch-resistant coating is recommended.
• Silicone nose pads with nonskid surfaces prevent glasses from slipping.
• Comfort cables secure frames by wrapping around the child’s ears and are available for children 1 to 4 years old. Straps are recommended for infants less than 1 year old and allow them to roll and lie down.
• Flexible hinges allow outward bending for easy removal by the child.
• Match the frame to the child’s facial shape and features to encourage compliance; if old enough, allow the child to choose the frames.
• To encourage compliance with infants and children, do not fight them when they remove glasses; be persistent, replace the glasses, and provide distraction. Parents may need to set the glasses aside for a few hours before trying again. Seek counsel from the prescribing provider for further help.
• Tinted lenses can be used for photosensitivity; ultraviolet (UV) light filters are helpful with aphakia (absence of lens), congenital absence of iris, and albinism.
• Do not place the glasses down with lenses in contact with hard surfaces.
• Clean glasses daily with liquid soap and a soft cloth (do not use paper products).
Contact Lenses
• Contact lenses are appropriate for children 8 years and older; children need to be able to demonstrate ability to manage lens hygiene, including insertion and removal.
• Contact lenses are helpful for an aphakic child who would otherwise need very thick glasses that distort images.
• Wear protective outer eyewear for sports.
• Do not wear contact lenses if one or both eyes are inflamed or when using topical ophthalmic medications. Children with recurrent conjunctival or corneal infections, inadequate tears, severe allergies, or excessive exposure to dust or smoke should not wear contact lenses.
• Omit wearing extended-wear contact lenses (usually worn overnight) for 1 night a week in order to perform lens hygiene procedures.
Ophthalmic Medications
Caution and precision must be exercised when administering ocular medications to children because their smaller body mass and faster metabolism may potentiate the action of the drugs and result in adverse ocular and systemic side effects. Topical ophthalmic medications, such as antibiotics, mydriatics, and corticosteroids, are frequently found in ointment or solution vehicles. These topical agents are primarily used for treating disorders affecting the anterior segment of the eye. Solubility is one of several factors that influence the absorption of topical ophthalmic medications. Those that are water soluble (e.g., anesthetics, steroids, and alkaloids) penetrate the corneal epithelium easily. Fat-soluble preparations (e.g., most antibiotics) do not penetrate the epithelium of the cornea unless it is inflamed.
Systemic Medications
In ocular infections involving the posterior segment and the orbit, systemic antibiotic preparations are necessary. A combination of topical and systemic antibiotics can also be used. In general, these conditions warrant referral to an ophthalmologist. Systemic drugs may also cause damage to the eyes (Table 28-5).
TABLE 28-5 Systemic Drugs, Herbs, and Nutritional Supplements That Can Cause Ocular Side Effects
| Drug | Ocular Side Effects | Intervention |
|---|---|---|
| Corticosteroids (prednisone at dosage of 15 mg/day for ≥1 year) | Cataracts, increased IOP | Monitor with ophthalmologic examinations. |
| Digoxin at moderately toxic ranges | Snowy, flickering, yellow vision | Resolves when drug is administered in correct range. |
| Isoniazid in greater than recommended dosages | Loss in color vision, decreased visual acuity, and visual field changes | Effects are reversible only if discovered early. Ophthalmologic examination is indicated before treatment and every 6 months; any changes warrant stopping isoniazid and referring to an ophthalmologist. |
| Isotretinoin | Pseudotumor cerebri (after initiating treatment) with resultant blurred vision, visual field loss, and varying visual acuity changes including optic neuritis, dry eye, decreased night vision, and transitory myopia | Monitor for symptoms. Annual eye exam recommended while on isotretinoin. |
| Minocycline hydrochloride | Pseudotumor cerebri and orthostatic blackouts, evidenced by blurred vision, visual field loss, varying visual acuity changes, diplopia; scleral pigmentation | Monitor for symptoms; scleral pigmentation may not resolve. |
| Phenytoin and carbamazepine | Blood levels in moderately toxic ranges can produce diplopia, blurred vision, nystagmus; sensitivity to glare | Resolve when therapeutic doses are within normal ranges. |
| Topiramate | Acute angle closure glaucoma; mydriasis; ocular pain; decreased visual acuity (myopia) | Onset of symptoms within 3-14 days after medication started. Stop medication. Treatment may include cycloplegics, hyperosmotic therapy, topical antiglaucoma medications. |
| Quetiapine | Cataracts | Monitor with ophthalmologic examinations. |
| Oral contraceptives (estrogen and/or progesterone) | Optic neuritis, pseudotumor cerebri, dry eyes | Monitor |
| Fluoxetine/SSRIs | Dry eye, blurred vision, mydriasis, photophobia, diplopia, conjunctivitis, and ptosis | Monitor |
| Herbs | ||
| Canthaxanthin (taken to produce artificial suntan; food coloring) | Decreased visual acuity; retinopathy | |
| Cassava with prolonged usage | Decreased visual acuity; retinopathy | Contains natural cyanide so it is important that this plant is processed correctly. |
| Datura (may be used by those with asthma, influenza, coughs) | Mydriasis | |
| Ginkgo biloba | Retrobulbar and retinal hemorrhage; hyphema | |
| Licorice | Decreased visual acuity | |
| Vitamin A | Intracranial hypertension | |
IOP, Intraocular pressure; SSRIs, selective serotonin reuptake inhibitors.
Data from Anderson AC: Ocular toxicology. In Shannon MW, Borron SW, Burns MJ, editors: Haddad and Winchester’s clinical management of poisoning and drug overdose, ed 4, Philadelphia, 2007, Saunders; National Registry of Drug-Induced Ocular Side-Effects: 2006 AAO syllabus. Available at www.piodr.sterling.net (accessed Jan 6, 2007); Reed Brandon, Hua Len: Potential ocular side effects of select systemic drugs. Faculty Scholarship, paper 3, 2010. Available at www.commons.pacificu.edu/cgi/viewcontent.cgi?article=1002&context=coofac (accessed Nov 14, 2010); Trobe J: The physician’s guide to eye care, San Francisco, 2001, The Foundation of the American Academy of Ophthalmology.
Eye Injury Prevention
• Children need to be instructed to:
 Use protective eyewear when hammering, using power tools or lawnmowers, or participating in a sport where there is a higher risk of ocular injury (see list under Sports Protection)
Use protective eyewear when hammering, using power tools or lawnmowers, or participating in a sport where there is a higher risk of ocular injury (see list under Sports Protection)• Parents further need to be instructed to:
 Limit and supervise the use of BB guns, air rifles, paintball devices, darts, and fireworks. The Prevent Blindness America (2008) organization does not support playing paintball games. At the very least, games should be supervised by a responsible adult and protective eyewear should be worn by participants.
Limit and supervise the use of BB guns, air rifles, paintball devices, darts, and fireworks. The Prevent Blindness America (2008) organization does not support playing paintball games. At the very least, games should be supervised by a responsible adult and protective eyewear should be worn by participants.Sunglasses
Ultraviolet (UV) A and UVB radiation from the sun can damage the lens and retina of the eye and cause cataracts and other conditions harmful to vision later in life (e.g., macular degeneration). Sunlight has more UVA than UVB, but UVB is more damaging. Sunglasses should be used to minimize such damage by absorbing these light wavelengths, even if wearing UV-treated contact lenses. It is never too early to start wearing sunglasses. Wearing a hat with a wide (3-inch) brim only cuts the radiation exposure in half.
Sports Protection
Protective eyewear should be properly fitted and selected specifically for the sport. A complete list of recommended eyewear for each sport is available online from the AAO website (www.aao.org). The list serves as a useful handout for parents. A headband or wraparound earpieces should be used to secure the glasses. Parents should only buy the protective eyewear certified by American Society for Testing and Materials (ASTM), the Hockey Equipment Certification Council (HECC), Canadian Standards Association (CSA), Protective Eyewear Certification Council (PECC), or National Operating Committee on Standards for Athletic Equipment (NOCSAE) for use in the particular sport. Fashion or street-wear glasses are inadequate, as is safety eyewear that carries an ANSI Z87.1 rating. Sports eye guards should have protective lenses designed to stay in place or pop outward in case of a blow to the eye (Prevent Blindness America, 2008).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree