chapter 7 Examining the Head and Neck
General Observations
Initial observations of facial features are important: Does the head look proportional to the face? Is the shape abnormal? Are the left and right sides of the face symmetrical? Are the eyes too close together or too far apart? Are the ears normally placed? Is the chin appropriately developed? Does the child look like the parents? The ability to describe visual observations is an essential clinical skill that takes practice to master. The range of “normal” in pediatric physical examination is extremely broad. Never, ever use offensive, demeaning terms such as “funny looking kid” to describe dysmorphic children. Describe the noted differences or asymmetries precisely. The child may look like a parent because they both have an autosomal dominant dysmorphic syndrome (see Chapter 5).
Approach to the Physical Examination of the Head
Examining the head
Head Shape
Craniosynostosis of the sagittal suture limits the skull’s width. As a result, compensatory excess growth occurs along the anteroposterior axis and possibly in the height of the skull, which produces a scaphocephalic shape, that is, a long, narrow skull (Fig. 7-1). Premature closure of the coronal suture results in a tall, wide head. When a suture closes prematurely, a palpable firm bony ridge sometimes is present along the suture line. Do not confuse this finding with normally overlapped sutures that are felt soon after birth.
Head Measurement
Accurate measurement of head circumference is surprisingly difficult. Measure the largest circumference possible by wrapping the tape around the most prominent parts of the forehead and occiput (Fig. 7-2). You should routinely take three measurements. If these measurements differ, you need to refine your technique. Even a slight variation in the position of the measuring tape changes the result significantly. Many infants and young children actively dislike head circumference measurement. Because a calm, cooperative child may become fretful, fearful, and oppositional when you attempt to obtain this measurement, it is best to leave it until the end of the examination. A parent’s assistance may be essential. I have found that the task is easier to accomplish when the infant is fed or cuddled and when the young child distracted with a toy or play activity.
The head circumference measurement must be plotted on a standardized head circumference graph. As with all standardized charts and graphs, no single value represents a “normal” head circumference (see Chapter 3). Measurements of new immigrants from various ethnic and racial groups may plot in the lower percentiles. Remember that, by definition, 3% of the normal population will have head circumferences that are below the third percentile or above the ninety-seventh percentile.
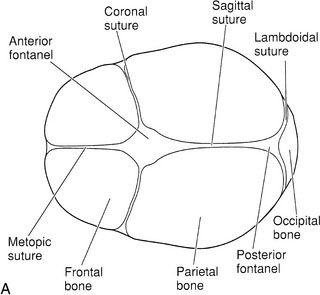
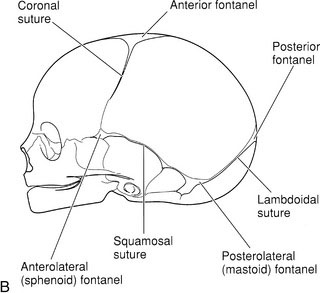
Fontanels
The fontanels are the gaps between bones in the infant skull where three skull bones meet (Fig. 7-2, A and B). Gentle palpation of the fontanels is a routine part of the newborn examination.
Increases in intracranial pressure, such as in meningitis, are reflected by changes in palpable tension of the fontanel and loss of normal venous pulsations (Fig. 7-3). A normal fontanel may feel full when the infant lays flat, cries, or struggles. It is best to assess anterior fontanel tension only when the infant is calm and held upright. With dehydration, the fontanel will appear sunken. Practice and palpation of dozens of fontanels will educate your fingers to detect abnormalities in size and tension. Each infant is his or her own standard. Serial assessments with careful descriptions of findings facilitate early detection of raised intracranial pressure.
Examining the ears
Hearing
Always ask parents if they have any concerns about their child’s ability to hear. Parents often suspect a hearing problem months before their child’s health care providers do. Audiologists are now able to measure hearing in infants from birth. The assessment of children with anomalies of the head and neck must always include formal hearing testing because the incidence of hearing problems is higher in children with such anomalies. Likewise, parental concerns about lags in language development should result in prompt audiologic evaluation. Delayed expressive language milestones may indicate hearing dysfunction (see Chapter 6).
Shape and Position
Start with a close inspection of the external ears. Are both present and normally formed, or do they fit the criteria for low-set ears? (See Chapter 5.) Do not be fooled by posteriorly rotated ears. If the vertical axis of the pinna is tilted posteriorly, the ear may appear to be low set. Minor anomalies of the ears such as skin tags, pits, or fistulas just anterior to the tragus are common and usually are of no major significance. Inspect and palpate the mastoid and postauricular areas. Gently move the pinna and tragus; any tenderness suggests otitis externa.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree