chapter 11 Evaluating Gastrointestinal Symptoms
Examination of the Abdomen
When examining a child with acute abdominal pain, it often is necessary to decide whether the child has a problem requiring surgery (i.e., an acute abdomen). Surgical disorders often present with a shorter history, and the most common cause of an acute abdomen in children is appendicitis. Disorders presenting with acute abdomen are discussed in more detail in Chapter 12.
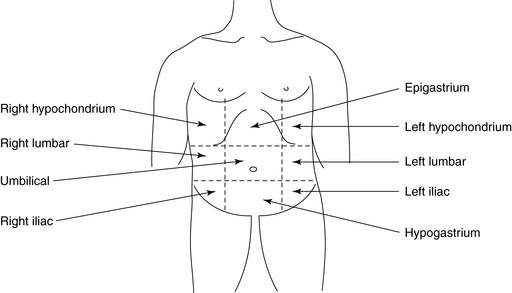
To describe the location of any abnormality, it helps to divide the abdomen into four quadrants with a horizontal line through the umbilicus and a vertical line from the xiphoid process to the symphysis pubis through the umbilicus. For infants and younger children with smaller abdomens, this division should suffice. For older children and adolescents, the abdomen can be divided into nine regions by including two additional vertical lines from the mid-clavicular area to the mid-inguinal point and two horizontal lines through the subcostal margins and the anterior iliac crests (Figure 11–1).
Palpation
The liver, spleen, and kidneys should always be palpated.
Liver
Always begin your palpation in the right iliac fossa so as not to miss the edge of a massively enlarged liver. The axis of your hand should be directed toward the right costal margin and at right angles to it. Rest your fingertips on the abdomen and gently depress them intermittently, without poking (Fig. 11–2). The child’s respiratory excursions will bring the liver down to make contact with the fingers (you don’t feel it; it feels you). One or both hands (one on top of another) may be used. Advance your fingers upward toward the costal margin in 1- to 2-cm increments.
Hepatomegaly can occur from many different causes, including:
Spleen
The spleen tip is palpable in about 10% of healthy children and often is palpable in newborns. In infants, the spleen enlarges downward toward the left lower quadrant, whereas in older children enlargement is toward the right lower quadrant. Palpation should begin in the right iliac fossa so as not to miss a very large spleen (Fig. 11–3). Be gentle, because an enlarged spleen could rupture if too much force is applied. Size should be recorded in centimeters below the left costal margin.
Kidneys
Kidneys are retroperitoneal and deep and are best palpated bimanually. With the child supine, place one hand in the renal (costovertebral) angle, beneath the twelfth rib and just lateral to the erector spinae (Fig. 11–4). Place your other hand anteriorly, just lateral to the rectus abdominis, in line with and parallel to the first hand. Ask the child to take a deep breath. Immediately at the end of inspiration, press your front hand firmly back against the other hand. A quick upward movement of the fingers of the hand in the renal angle is made (ballottement), and the kidney is trapped between the two hands. Unless the kidney is massively enlarged, successful renal palpation requires considerable experience. The percussion note over the kidney will be resonant because of overlying intestine, which helps differentiate it from the spleen or liver.
Rectal Examination
In older children, a rectal examination is best performed with the child in the left lateral position with the spine and knees fully flexed. Infants and younger children can be examined in a knee-chest position. The examination should be conducted systematically. Presence of stool in the underwear implies fecal incontinence, most likely from encopresis. Examine the perianal area for excoriations, skin tags, or fistulae. Sentinel skin tag(s) overlying a chronic anal fissure in older children are pathognomonic of Crohn’s disease (Fig. 11–5). The buttocks should be gently spread to look for any anal fissure. Acute anal fissures occur from passage of large, very hard stools. Digital rectal examination in such cases is painful and unnecessary. Acute anal fissures often are difficult to view because there is considerable spasm of the anal sphincters, and the child does not relax enough for good visualization. The diagnosis is best made by history.
< div class='tao-gold-member'>