Symptoms
1. Nasal
Unilateral nasal obstruction (70 %)
Epistaxis (50 %)
Unilateral nasal mass
Rhinorrhea
Anosmia (5 %)
2. Neurologic
Headaches
Cranial nerve paralysis
3. Ophthamologic
Proptosis
Visual disturbance
Excessive lacrimation
4. Facial
Facial pain/swelling
Parathesia (rare)
5. Cervical
Neck swelling (5–7 % at diagnosis)
Evaluation
Examination
A full otolaryngologic and cranial nerve examination should be performed. This should include nasal endoscopy. ENB does not have specific distinguishing features on examination but usually appears as a unilateral polypoid, glistening, soft, red–grey mass with intact mucosa arising in the upper nasal cavity that often bleeds easily on instrumentation. Cervical lymphadenopathy may be palpable in advanced disease. Ectopic tumors within the paranasal sinuses are rare, but have been described in the sphenoid sinus, lateral nasal wall, petrous apex, maxillary sinus, and the nasopharynx [5]. Diagnosis is made via biopsy, which should not be performed until imaging studies are complete. General anesthesia is recommended for biopsy, due to the highly vascular nature of the tumor; a comprehensive endoscopic examination can also be performed at the same time.
Differential Diagnosis
All causes of pediatric sinonasal masses must be carefully excluded (Table 17.2).
Table 17.2
Differential diagnosis of ENB
Infectious/inflammatory | Fungal rhinosinusitis |
Inflammatory polyp | |
Adenoidal hypertrophy | |
Wegners’ granulomatosis | |
Congenital masses | Dermoid cyst |
Glioma | |
Encephalocoele | |
Teratoma | |
Primary neoplasms | Rhabdomyosarcoma |
Nasopharyngeal carcinoma | |
Squamous cell carcinoma | |
Sinonasal undifferentiated carcinoma | |
Lymphoma | |
Angiofibroma | |
Osteosarcoma | |
Chondrosarcoma | |
Ewing sarcoma / PNET | |
Neuroblastoma | |
Idiopathic midline granuloma | |
Meningioma | |
Hemangioma | |
Hemangiopericytoma | |
Fibrosarcoma | |
Fibrous histiocytoma | |
Malignant melanoma | |
Neuroendocrine carcinoma | |
Secondary neoplasms | Metastases |
Chordoma | |
Meningioma | |
Lymphoma |
Histopathology
ENB is histologically very similar to small, round, blue cell tumors. These are important to distinguish, as they respond very differently to different treatment modalities (Fig. 17.1). Tumor cells are “small, round, blue” and mitotically active. The hallmark of well-differentiated ENB is small, round neuroepithelial cells arranged in rosettes (Flexner-Wintersteiner) or pseudorosettes (Homer-Wright) patterns, separated by fibrous elements. Rosettes consist of a central space ringed by columnar cells. Immunohistochemical tests are helpful in differentiating neuroblastomas from other malignant small round cell tumors, however, to date there is no test specific to ENB.[6] (Table 17.3).
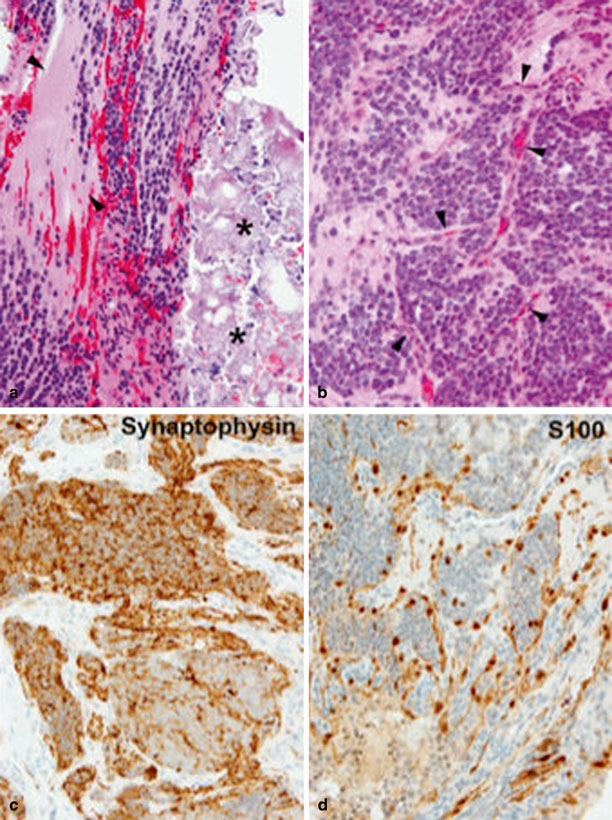
Fig. 17.1
Olphatory neuroblastoma. a Poorly differentiated ENB with abundant neuropil (between arrowheads) and a low mitotic/karyorrhectic index. Extensive dystrophic calcifications are seen on the right (asterisks). b Tumor cells are arranged in tight nests outlined by a delicate capillary network (arrowheads). c Tumor cells are strongly and diffusely immunoreactive for synaptophysin. d A network of Schwannian sustentacular cells strongly immunoreactive for S100 protein invests nests and cords of tumor cells
Table 17.3
Immunohistochemical features of ENB and other sinonasal tumors
Immunohistochemistry | Other tests | |
|---|---|---|
ENB | Positive for S-100, neuron-specific enolase (NSE), synaptophysin, NFP, CD56, chromogranin | Ki-67 positive—high proliferation index |
Negative for cytokeratin, vimetin, desmin, myogenin, common leukocytic antigen (CD 45RB), CD99 (MIC2 antigent) | ||
Neuroblastoma | Positive synaptophysin, Leu7, neurofilament protein, NSE | Elevated catecholamines |
Rhabdomyosarcoma | Positive for desmin, muscle-specific actin, myoglobin | Loss of chromosome 11 |
Lymphoma | Positive for C45 | |
Ewing sarcoma | Positive for MI22/CD99 | 11:22 translocation |
Malignant melanoma | Positive for S-100, MART-1/Melan-A, HMB-45 |
Imaging Studies
Both computed tomography (CT) and magnetic resonance imaging (MRI) are recommended for the workup of ENB. Particular attention needs to be paid to areas such as the lamina papyracea, the fovea ethmoidalis, and the cribriform plate.
CT Imaging
A fine-cut CT with contrast, according to an image guidance protocol, should be performed. ENB appears as a homogeneous soft tissue mass with uniform enhancement on contrast (Fig. 17.2). Nonenhancing areas may suggest areas of necrosis. Speckled calcifications may also be present. CT is useful to evaluate for bony erosion, especially of the lamina papyracea, cribiform plate, and fovea ethmoidalis. A “dumbbell-shaped” mass extending across the cribriform plate is one of the most characteristic findings on imaging for an ENB.
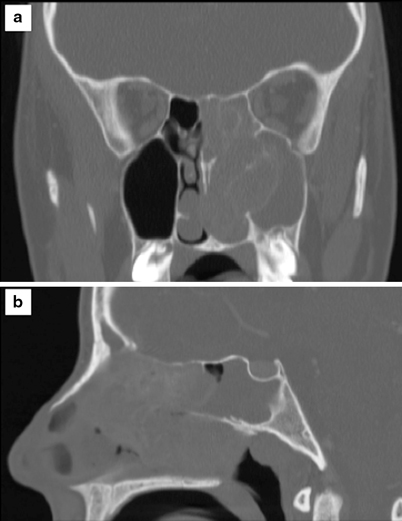
Fig. 17.2
A coronal (a) and axial (b) postcontrast CT image of the paranasal sinuses in a 16-year-old girl who presented with a 6-week history of nasal obstruction. A large heterogeneously enhancing soft tissue mass completely fills and opacifies the left maxillary antrum. There is thinning of the bony margins of the sinonasal cavity and left maxillary sinus consistent with areas of bone resorption . The left lamina papyracea is thinned but intact. The tumor abuts the skull base but there is no evidence of soft tissue extension into the anterior cranial fossa. Biospy of this tumor was consistent with an ENB
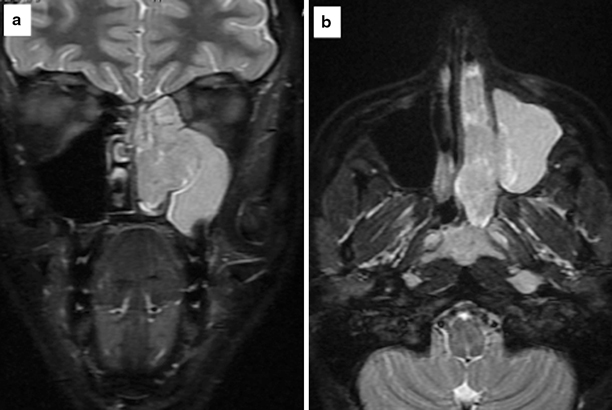
Fig. 17.3




A coronal (a) and axial (b) T1-weighted post gadolinium MR image of the same patient in Fig. 17.1, showing a multilobulated solid mass centered in the left nasal cavity that extends laterally into the left maxillary sinus, cephalad into the ipsilateral ethmoid sinus, and posteriorly into the nasopharynx. Retained left maxillary secretions are seen in the coronal image. There is no evidence of intraorbital or intracranial extension
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


