CHAPTER 8 Esophageal Replacement
Colonic Interposition
Step 1: Surgical Anatomy
♦ Preservation of the lower esophageal sphincter is ideal; the colonic interposition conduit should bridge the defect in a course that is straight and as short as possible to encourage dependent drainage.
♦ The portion of the colon to be used for esophageal replacement depends largely on the length required. Anatomic considerations could determine whether colonic interposition is possible or an alternative should be used; prior symptomatic short colon could cause exacerbation of intestinal problems if used as a conduit.
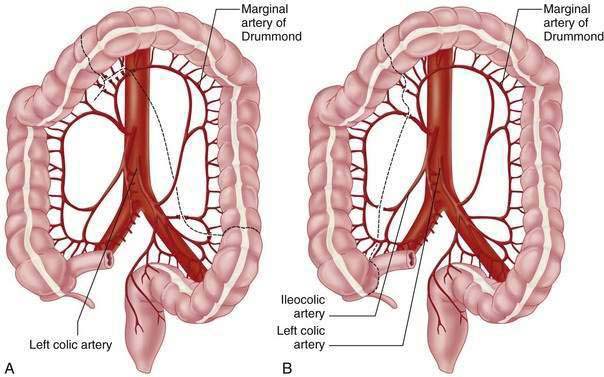
♦ An isoperistaltic conduit consisting of transverse and descending colon in the left hemithorax in the retrohilar position is best suited for long-gap esophageal atresia. Vascular supply is based on the left colic artery and collaterals from the marginal artery of Drummond to the transverse colon (Fig. 8-1, A).
♦ An alternative conduit is the ascending or transverse colon segment based on the ileocolic and middle colic artery, respectively (Fig. 8-1, B).
Step 2: Preoperative Considerations
♦ Before any replacement procedure is done, a thorough radiologic evaluation of the stomach and gastrointestinal tract is essential.
Step 3: Operative Steps
Incision
♦ Gastrocolic ligament is divided to free the transverse colon. Descending and sigmoid colon are mobilized by dividing lateral peritoneal attachments.
♦ Mesentery of the transverse and descending colon is incised by dividing the left branch of the middle colic artery and preserving the marginal arcade and the left colic artery and its arcades (see Fig. 8-1, A).
♦ The phrenoesophageal ligament is incised; dissection of the esophagus along the hiatus, gastroesophageal junction, and into the mediastinum is performed.
♦ The length of the colon conduit is determined, and then the colon is divided into the transverse and descending regions, retaining the left colic blood supply. If the right colon is used as the conduit, the ileocolic vessels are preserved (see Fig. 8-1, B).
♦ A left lateral thoracotomy (through the 5th and 6th intercostal spaces) is done to give access to the chest for further dissection of the esophagus and subsequent placement of the colonic conduit.
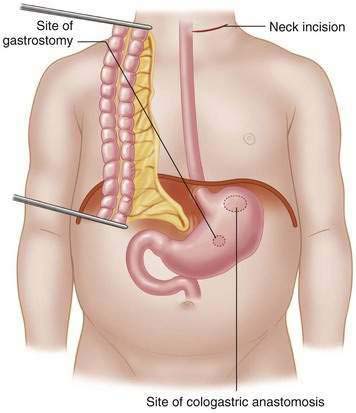
♦ Figure 8-2 demonstrates the configuration of the colon conduit before placement in the retrohilar or substernal position.
♦ The colonic segment and its pedicle are brought anterior to the pancreas behind the stomach and through an incision made in the gastrohepatic ligament and then passed through the esophageal hiatus or through a lateral incision in the diaphragm. The retrohilar tunnel is created lateral to the descending aorta behind the aortic arch.
♦ The upper end of the colonic segment is brought through Sibson fascia posterior to the subclavian vessels and lateral to the carotid sheath. Figure 8-3, A provides a lateral perspective of the colon conduit.
♦ If a retrohilar approach is not possible, the colonic conduit can also be positioned retrosternal (Fig. 8-3, B).
♦ A delayed proximal anastomosis may be indicated if the blood supply of the cervical portion of the conduit is marginal. This can be performed several weeks later.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree