41 Environmental Health Issues
• Some providers may believe the effect of environmental agents is negligible, that lifestyle choices, genetic conditions, and/or infectious agents are responsible for most disease.
• There is not always definitive evidence that exposure to an environmental agent causes a particular disease. Is the condition being seen clinically caused by environmental exposure or something else?
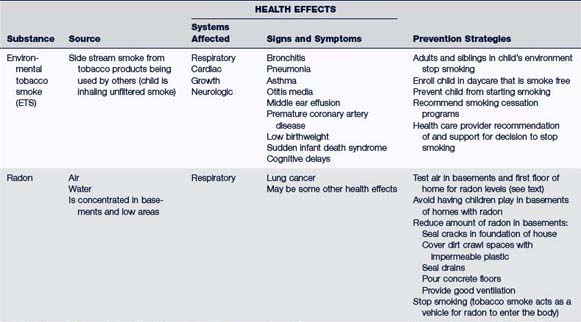
• Exposure to some environmental agents may cause disease if there are preexisting or genetic conditions, or agents working together may cause problems (e.g., tobacco smoke and radon combined). It is often difficult for the provider to sort out the many variables.
• Research findings vary as to the type of problem caused by an environmental agent. What effect does an environmental agent have on the human body? Using the Multiple Exposure-Multiple Effects model (Briggs, 2003), some agents can cause several problems, and many different agents may cause the same problem (e.g., cancer). Sometimes the effect may be so subtle as to be missed: a decline in IQ scores after exposure to lead may still leave the child within the range of “normal” IQ.
• To what environmental agents has this individual been exposed? When? The health effect of an agent may be delayed for years and the exposure forgotten or unnoticed at the time it occurred (e.g., asbestosis, melanoma).
• Some providers may believe that correcting environmental health problems is beyond their purview. Exposure to disease-causing agents, they think, is a systemic not an individual issue, so beyond treating the illness, they may feel they can do nothing to help their patients or change the system.
• Providers feel inadequate to the task; they are not prepared well to manage environmental health concerns. Many providers state they lack knowledge and confidence in managing children’s environmental health issues, failing, for example, to know about and use available resources (e.g., the Pediatric Environmental Health Specialty Unit [PEHSU] in their region) (Trasande et al, 2010). Nursing and medical schools do not devote sufficient time to teaching about environmental health, and continuing education may be limited.
The current situation is grim, but it is important to note that health care providers are increasingly aware of the problem, and many efforts are being made to address environmental health in pediatric practices. A network of regional PEHSUs has been created to provide information, clinical consultation, and support for pediatric providers (see www.aoec.org/PEHSU.htm). In 1999, the American Academy of Pediatrics (AAP) published a pediatric environmental health manual for providers (Etzel and Balk, 2003). Educators are developing curricula and preparing materials for students in health disciplines (Beitz and de Castro, 2010; Jamil et al, 2010); some are suggesting a medical specialty in environmental medicine (le Moal and Reis, 2011), and tools for assessment and management of environmental variables continue to be written (Cohen Hubal et al, 2010; Judson et al, 2008; Kavlock and Dix, 2010). New technology allows for more sophisticated assessment of how chemicals affect the human body, and intricacies of the environment-health relationship are better understood. Lack of strong evidence for a cause-effect relationship is not due to absence of an effect; rather, more research is needed to clearly establish the connections (Wigle et al, 2008). In 2000, the U.S. Congress authorized the National Children’s Study to investigate the root causes of many childhood and adult diseases. It is proposed that 100,000 children be followed from before conception until 21 years old, examining environmental influences on health, including diet, ambient air, and home and school environments as well as interactions with various genetic traits. As of 2010, 37 regional participation sites had been identified; the challenge is to develop a recruitment plan, assessment tools, and protocols to coordinate, administer, and conduct the research (Savitz and Ness, 2010).
 Principles for Understanding Children’s Environmental Health
Principles for Understanding Children’s Environmental Health
Children’s Increased Risk for Environment-Related Illness
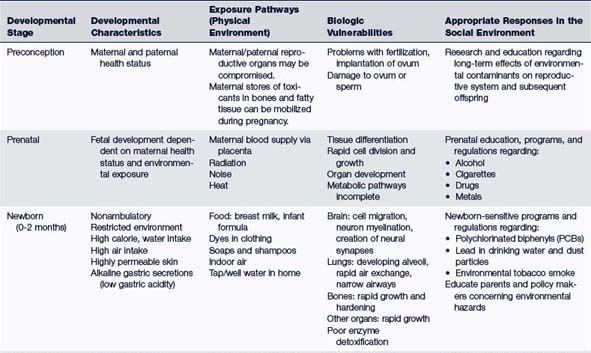
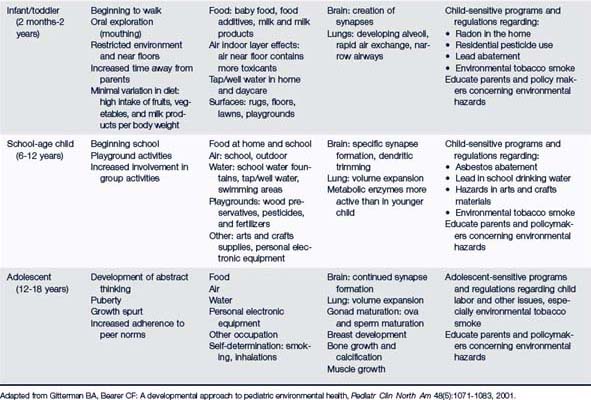
Children, because of their developmental immaturity, rapid growth, size, and behavior, are particularly susceptible to environmental threats (Table 41-1). Exposure to toxins or other harmful substances affects growth and damages organs or body systems during critical developmental periods or windows of vulnerability, prenatally and during childhood. It is known, for instance, that a 50-mg dose of thalidomide, administered during the 26th day of gestation will likely result in major malformations to an embryo but that same dose taken at the 10th week of gestation will have no effects (Brent, 2004). Toxicants that cross the placenta (e.g., drugs, carbon monoxide [CO], mercury, lead, and cotinine [from environmental tobacco smoke]) can contribute to low birthweight, spontaneous abortion, intrauterine growth retardation, increased risk of cancer, poor cognitive and behavioral development, and birth defects. Approximately 3% of all babies born in the U.S. have a serious birth defect. The rate of some birth defects is increasing (Brent, 2004), and about 10% appear to be related to environmental exposure (Chervenak et al, 2010).
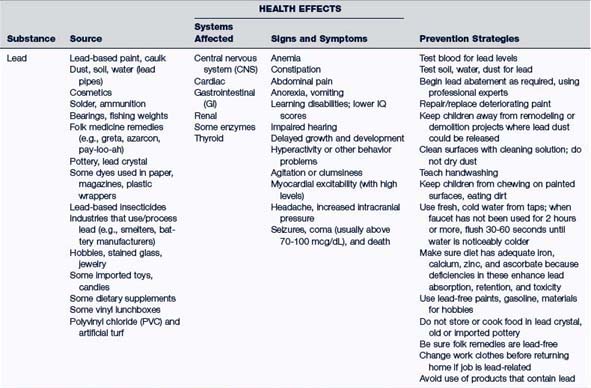
Epidemiologic Model: Risk Assessment Approach
A first step in an epidemiologic approach (Fig. 41-1) identifies the interactive factors in the environment, including receptors (i.e., hosts or living things that are susceptible or exposed to environmental agents); toxins, or harmful substances that might cause damage (i.e., the agent); and the environmental medium, or route by which exposure could occur (e.g., air, water, or food).
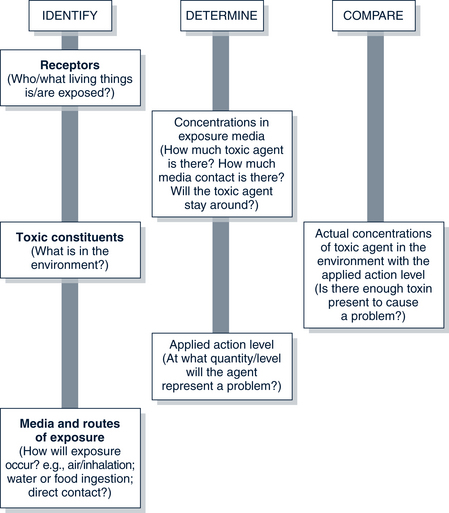
FIGURE 41-1 Risk assessment of environmental hazards.
(Adapted from Oregon Poison Center and Health Division, Oregon Department of Human Resources: Environmental hazards in perspective: seminar syllabus and environmental health resource notebook, Portland, 1994, Oregon Department of Human Resources.)
• How susceptible is the receptor to the agent (e.g., age, sex, genetics, diet, and general health)?
• At what quantity (i.e., dose) will the agent present a problem or cause a response in this receptor? This amount is called the applied action or dose-response level. For some agents, any exposure represents a risk.
• What is the concentration of the toxic agent? How much is there? How strong is it? How long will it stay around? What is the extent of contact of the toxic agent with the receptor?
Toxicologic Principles
Distribution
Toxic agents are distributed throughout the organism via the blood or lymph systems. The ability of an agent to cross the blood-brain barrier, the amount of blood flow to an organ, and the affinity of tissues to take up a particular agent (e.g., lipid-soluble chemicals are found in fatty tissues) all influence the degree to which a toxicant will be distributed throughout the body.
 Primary Care Approach to Children’s Environmental Health
Primary Care Approach to Children’s Environmental Health
Assessment
Assessment of environmental health hazards should be integrated into regular health appraisals, as well as examinations of ill children. Figures 41-2, 41-3, and 41-4 list essential questions to ask for an environmental history, including questions related to asthma.
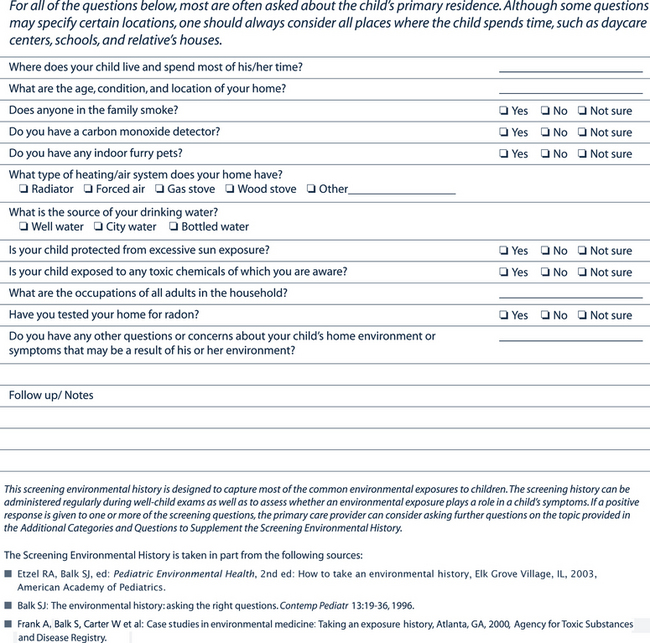
FIGURE 41-2 Pediatric environmental history (0 to 18 years of age): The screening environmental history.
Used with permission of the National Environmental Education Foundation, Washington, DC. Available at www.neefusa.org/pdf/PedEnvHistoryScreening/pdf (accessed Apr 4, 2011).
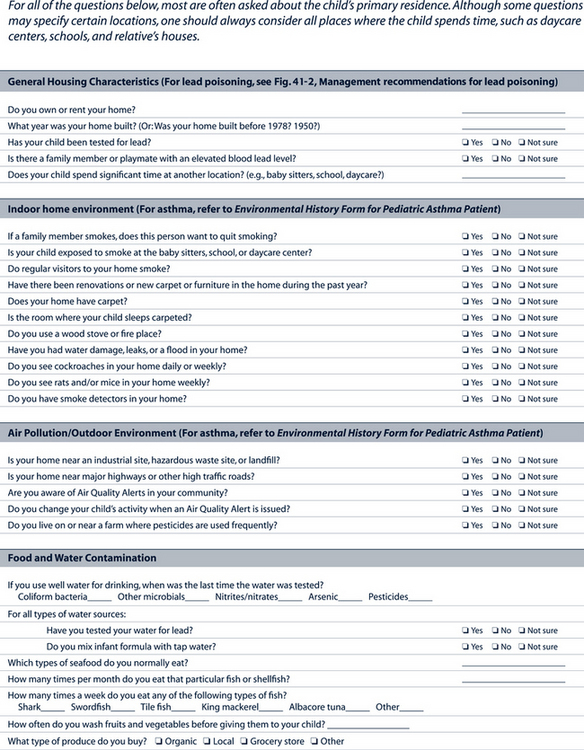
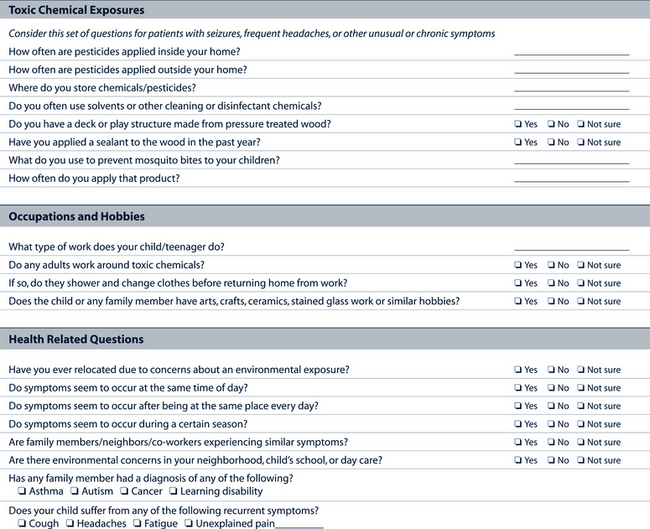
(Used with permission of the National Environmental Education Foundation, Washington, DC. Available at www.neefusa.org/pdf/PEHIhistory.pdf. Accessed April 4, 2011.)
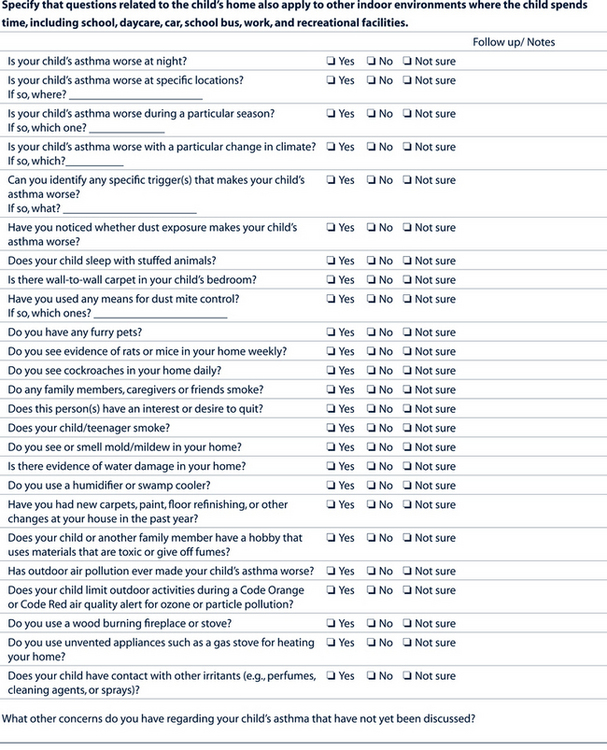
FIGURE 41-4 Environmental history form for pediatric asthma patient.
(Used with permission of the National Environmental Education Foundation, Washington, DC. Available at www. neefusa.org/health/asthma/historyform/htm. Accessed December 1, 2011.)
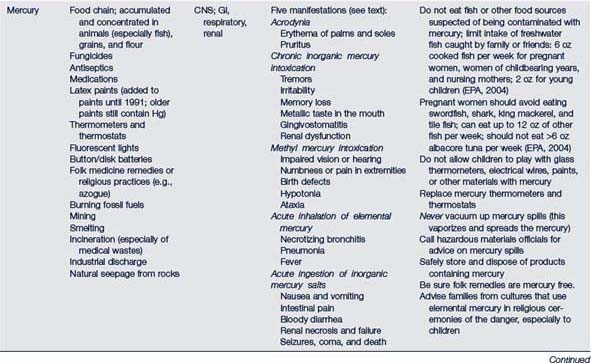
Physical Examination
The physical examination should cover all body systems thoroughly. Evaluate agent-specific findings (e.g., burns caused by chemicals and neurotoxicity caused by mercury), but also look for subtle, nonspecific signs and symptoms (e.g., skin rashes and headaches). The effects of toxicants on the body can be subclinical in many cases, and effects can occur long after exposure.
Diagnostic Studies
• For most toxins, valid and reliable tests have not been developed.
• For those toxins that do have tests, not all laboratories are capable of performing them. The provider should consult with individual laboratories regarding their capabilities.
• Many tests show a wide range of reference levels at which “toxicity” appears.
• There may be little correlation between exposure and levels present in the body at the time the test is done. Levels may have returned to normal, despite damage done to the body; or a one-time sample can reflect recent active exposure, but not measure the total body burden of the contaminant.
Some available tests include the following:
• Gas-liquid chromatography (for PCBs)
• Atomic absorption spectrometry (for mercury)
• Carboxyhemoglobin (for CO poisoning)
• Twenty-four-hour urine (for heavy metals)
• Urinary cotinine assays (for tobacco metabolites)
• Plasma cholinesterase (ChE) levels (for pesticide metabolites, organophosphates)
Management of Environmental Conditions
Primary Prevention
Primary prevention also takes place at the public policy level. Regulations or legal restrictions can prevent health problems (e.g., through implementation of air and water quality standards, restaurant and food handling regulations, or bans on the use of hydrofluorocarbons). Various U.S. federal agencies function to regulate development and use of hazardous materials (e.g., the EPA, the U.S. Consumer Product Safety Commission, and the Occupational Safety and Health Administration [OSHA]). In 1997, the U.S. joined seven other countries (the G-8) in creating the 1997 Declaration of the Environment Leaders of the Eight on Children’s Environmental Health, raising the issue of protection of children from environmental threats to an international level (EPA, 1997).
 Common Environmental Agents and Adverse Effects
Common Environmental Agents and Adverse Effects
General Pediatric Poisoning
Assessment (Rodgers et al, 2007)
History
• Type of substance taken in. Name of product and ingredients from label
• Exact time of intake or exposure
• Reaction or signs and symptoms and their progression over time
• Child’s health status before poisoning (e.g., any significant chronic illness? Is child taking prescription medication?)
• Contact information including phone and address if the assessment is via phone
Differential Diagnosis
A history of exposure distinguishes poisoning or potential poisoning from acute-onset illness. Because there is not always an obvious episode of exposure, the provider should be suspicious of poisoning in otherwise well children who experience sudden seizures, GI distress, or cardiorespiratory collapse.
Management
Basic decontamination guidelines for contact contaminants are listed in Box 41-1. Prompt action to remove the toxin from the skin (e.g. insecticide exposure) or from the eye may prevent major absorption. With ingested toxins, most liquid products are absorbed completely within 30 minutes and solids within 1 to 2 hours. Thus timing is critical, and because decontamination procedures also contain risks, one must consider whether the technique chosen is likely to be of sufficient value to merit its use. Activated charcoal, an adsorbent agent, has been demonstrated to have good efficacy for many, but not all, toxins. The toxins adhere to its surface, rather than being absorbed from the GI mucosa. The use of gastric lavage is coming into question more and more because it only removes a small portion of gastric contents. Syrup of ipecac is not recommended for use in poisoning (American Academy of Pediatrics [AAP], 2003; Rodgers et al, 2007). Cathartics are often used with activated charcoal but without good evidence to support use. Whole-bowel irrigation with a polyethylene glycol electrolyte into the stomach to cleanse the entire GI tract has been shown to be somewhat successful for substances that are absorbed slowly, such as iron or sustained-release medications (Rodgers et al, 2007).
BOX 41-1 Basic Decontamination Protocol
• Determine the need for decontamination by calling the poison control center in your area.
• If clothing has been contaminated, strip the patient and double-bag clothing, then flush the entire body with plain water for 2 to 5 minutes. If contaminated with dust, keep clothing dry; remove carefully to minimize dust becoming airborne; if possible, apply dust mask or respirator to patient before removing clothing (brush dust from face first).
 Irrigate eyes with sterile saline, balanced salt solution, or Ringer’s lactate for at least 15 to 30 minutes.
Irrigate eyes with sterile saline, balanced salt solution, or Ringer’s lactate for at least 15 to 30 minutes. Wash appendages (if that is only body part contaminated) without wetting the whole body, if possible.
Wash appendages (if that is only body part contaminated) without wetting the whole body, if possible.• Oily or greasy contamination
Lead
Description
Children and adults differ in lead exposure sources, absorption, metabolism, and specific ways in which toxicities are expressed. Children are more likely to be exposed via hand-to-mouth behaviors; the fraction of lead absorbed from the gut is higher in infants and children, and the amount absorbed increases in children when nutritional deficiencies, such as iron and calcium, are present. Temporary peripheral neuropathies from lead toxicities predominate in adults, whereas permanent central nervous system effects predominate in children. If children have higher BLLs at age 6 years than they did at age 2 years, they are more likely to have IQ deficits and behavior problems than children who have a higher BLL at age 2 than at age 6 (Hornung et al, 2009).
Epidemiology
The major source of lead poisoning in children is dust and chips from deteriorating paint on interior surfaces. Before 1950, much white house paint was 50% lead and 50% linseed oil. Limits on the lead content of paint began in 1955 and were augmented in 1971 and 1977. The prevalence of lead hazards in homes built before 1960 is five to eight times greater than in homes built between 1960 and 1977, and 14 to 23 times greater than in homes built between 1978 and 1998 (Jacobs et al, 2002). Children are at greatest risk in houses where paint is peeling or those where renovation with paint removal is occurring. Lead dust is more readily absorbed than chips. Soil near deteriorating homes, mines, lead-using industries, and smelters can have high lead levels. Acidic water with low mineral content can leach lead from lead pipes or solder. Hot water leaches more lead than cold. Brass fixtures also contain lead. Food can be a source of lead. For example, lead from soil can contaminate root vegetables. Some other sources of lead are listed in Table 41-2. Lead crosses the placenta so that the fetal and newborn blood level is close to that of the mother’s, but little lead is transferred in breast milk.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree