Chapter 32 Enuresis/Urinary Incontinence
ETIOLOGY
What Causes Incontinence?
Table 32-1 lists causes of primary and secondary incontinence. Primary enuresis, especially primary nocturnal enuresis, is thought to result from a physiologically immature bladder and resolves with time. Incontinence, either primary or secondary, can be caused by anatomic abnormalities of the urinary tract or spine or by other serious conditions that cannot be excluded without further evaluation, including functional abnormalities of the bladder, bladder inflammation, or polyuric states. History and physical examination provide critical information regarding the distinctions between these conditions. Secondary enuresis that results from psychological stressors is a diagnosis of exclusion.
Table 32-1 Causes of Incontinence
| Primary Incontinence | Secondary Incontinence |
|---|---|
| Physiologic (primary enuresis) | Psychological stressors (secondary enuresis) |
| Anatomic abnormalities (ectopic ureter, neurogenic bladder) | Anatomic abnormalities (neurogenic bladder) |
| Bladder irritation (urinary tract infection, hypercalciuria) | |
| Polyuria (diabetes mellitus, diabetes insipidus, polydipsia, diuretic use) | |
| Bladder dysfunction (bladder sphincter dyssynergia) |
What History Identifies the Cause of Incontinence?
A detailed history must focus on the child’s voiding pattern and frequency. The pattern of incontinence is also important: diurnal, nocturnal, or both; constant dribbling or intermittent enuresis. Constipation often accompanies enuresis. Specific inquiry about social stressors should be made. History suggestive of diabetes (Chapter 60) or urinary tract infection (Chapter 65) will direct specific investigations. Urgency, dysuria, or family history of kidney stones will prompt evaluation for hypercalciuria. Family history is often positive in primary enuresis. Physical examination must include careful evaluation of the back for sacral or spine abnormalities, including hair tufts, masses, or deep sacral dimples. Genitourinary abnormalities, and neurologic problems, especially of the lower extremities, must be identified if present. Rectal examination to assess tone and presence or absence of constipation is important.
What Testing Is Needed?
 Random urine specimen for calcium-to-creatinine ratio for hypercalciuria
Random urine specimen for calcium-to-creatinine ratio for hypercalciuria
 Blood glucose concentration for diabetes
Blood glucose concentration for diabetes
 Kidney-ureter-bladder (KUB) radiograph and kidney and bladder ultrasound for spine abnormalities and neurogenic bladder
Kidney-ureter-bladder (KUB) radiograph and kidney and bladder ultrasound for spine abnormalities and neurogenic bladder
 Voiding cystourethrogram and intravenous pyelogram to look for bladder and ureteral anomalies
Voiding cystourethrogram and intravenous pyelogram to look for bladder and ureteral anomalies
TREATMENT
How Do I Treat Incontinence?
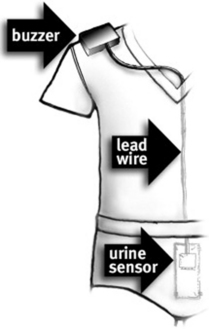
Incontinence is a symptom and not a disease. Therefore management must address the underlying cause. For children with primary nocturnal enuresis, continued reassurance to the child and the family is imperative. Enuresis will resolve with time as the bladder matures. Motivated children whose quality of life is significantly hampered by their bedwetting may benefit from a commercially available enuresis alarm (Figure 32-1). Alarms are associated with a sustained reduction in enuresis even after they are discontinued. While awaiting spontaneous resolution, the intermittent use of nasal or oral desmopressin will allow older children to participate in overnight social outings without embarrassment. This is purely a symptomatic treatment and does not hasten bladder maturation; most children relapse when the medication is stopped.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree