ENDOCRINE
What is the most likely diagnosis?
a. Pituitary adenoma
b. Intracranial hemorrhage
c. Meningioma
d. Cavernous venous thrombosis
e. Testicular cancer
Answer a. Pituitary adenoma
Pituitary adenoma most often presents with symptoms of hormonal excess. The most common pituitary lesion is a microadenoma. In this patient, decreased libido, gynecomastia, and ED are consistent with prolactinoma. Intracranial hemorrhage, cavernous thrombosis, and meningioma would present with focal neurologic deficits in addition to the visual deficits. Testicular cancer presents with enlarged testicle, and there is no functional abnormality. Testicular cancer does not interfere with hormone function.
Bitemporal visual field defects are caused by compression of the optic chiasm.
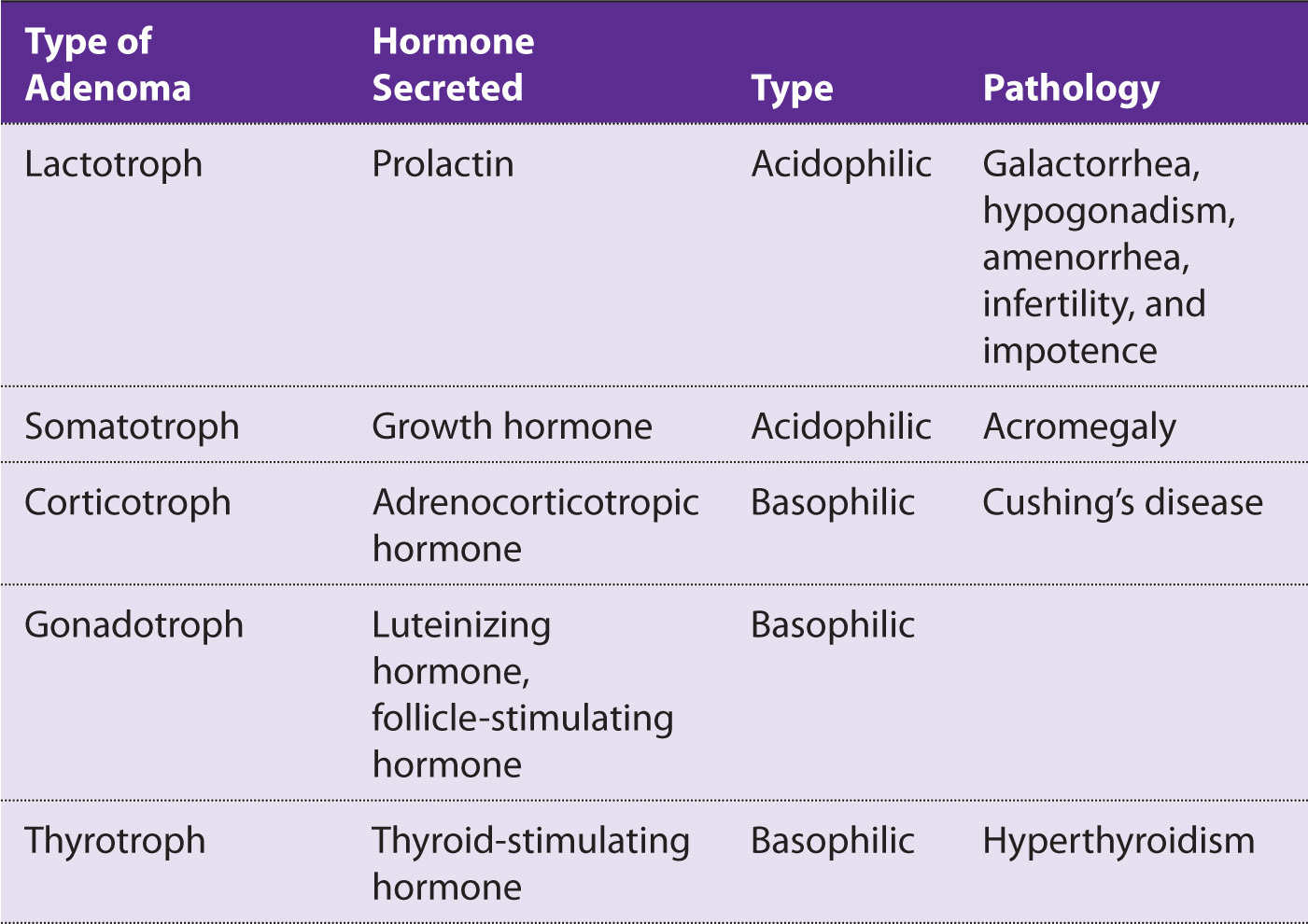
The most common pituitary adenoma is a prolactinoma (Table 6-1).
Table 6-1 Types of Adenomas
Prolactin inhibits follicle-stimulating hormone, luteinizing hormone, and gonadotropin-releasing hormone.
What is the best next step in the management of this patient?
a. Serum thyroid-stimulating hormone (TSH) level
b. Serum prolactin level
c. Magnetic resonance imaging (MRI)
d. Serum testosterone level
e. Serum insulin-like growth factor-(IGF)1
Answer b. Prolactin level
The best initial test to diagnose a patient with signs and symptoms of prolactinoma is to check the serum prolactin level. Serum TSH would be used to confirm if a patient has a rare TSH-secreting tumor. Serum testosterone can be measured because hypogonadism presents with ED and decreased libido. Because of gynecomastia, a pituitary source must be given first consideration. Serum IGF-1 level is used in patients who present with acromegaly. MRI is never the first step in an endocrinologic disorder. MRI is used to confirm a mass lesion if serum levels of a particular hormone are elevated. If prolactin levels are elevated, then the most accurate test is an MRI of the brain to look for a mass lesion in the hypothalamic–pituitary region.
Do not measure prolactin levels after a breast examination because manipulation causes a modest rise in prolactin levels.
Prolactinoma presents with amenorrhea and galactorrhea in women. Check a pregnancy test first before proceeding.
If a patient is taking one of these drugs that cause hyperprolactinemia, it must be discontinued:
• Haloperidol
• Risperidone
• Olanzapine
• Desipramine
• Metoclopramide
• Verapamil
• Morphine
Antipsychotic medications inhibit prolactin.
During pregnancy, the pituitary gland doubles in size and prolactin levels increase by 10-fold during this period.
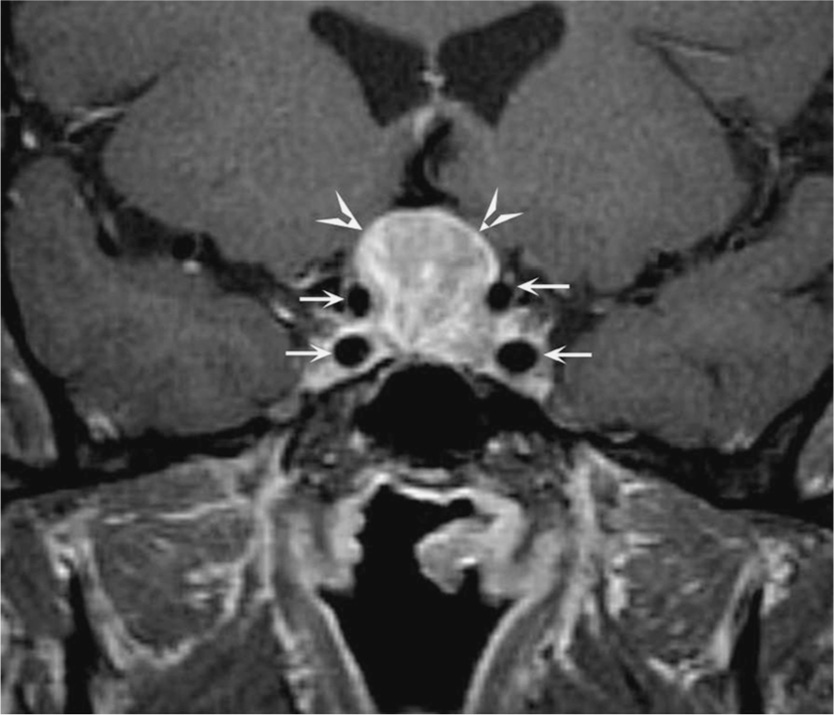
Figure 6-1. Coronal T1-weighted postcontrast magnetic resonance image shows a homogeneously enhancing mass (arrowheads) in the sella turcica and suprasellar region compatible with a pituitary adenoma; the small arrows outline the carotid arteries. (Reproduced, with permission, from Longo DL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.)
What is the best next step in the management of this patient?
a. Cabergoline
b. Benztropine
c. Baclofen
d. Beclomethasone
Answer a. Cabergoline
Cabergoline and bromocriptine are dopamine agonists that are first-line therapy to shrink the size and secretory potential of prolactinomas. Benztropine (an anticholinergic), baclofen, and steroids have no role in the treatment of prolactinoma. Many patients cannot tolerate bromocriptine because of nausea. This is why cabergoline is indicated.
Serum prolactin levels and adenoma size typically improve within 2 to 4 weeks of therapy with a dopamine agonist.
Dopamine inhibits prolactin release.
Surgery is used when dopamine agonist therapy does not work. Women who wish to become pregnant and have a prolactin-secreting tumor larger than 3 cm should have surgery.
The type of intervention is transsphenoidal surgery, which occurs via an incision in the upper lip into the brain.
High calcium inhibits neural depolarization.
Calcium increases gastrin release. Gastrin produces acid from parietal cells.
PTH lowers phosphorus level by increasing proximal tubule excretion.
What is the most likely diagnosis?
a. Primary hyperparathyroidism
b. Secondary hyperparathyroidism
c. Tertiary hyperparathyroidism
d. Vitamin D toxicity
Answer a. Primary hyperparathyroidism
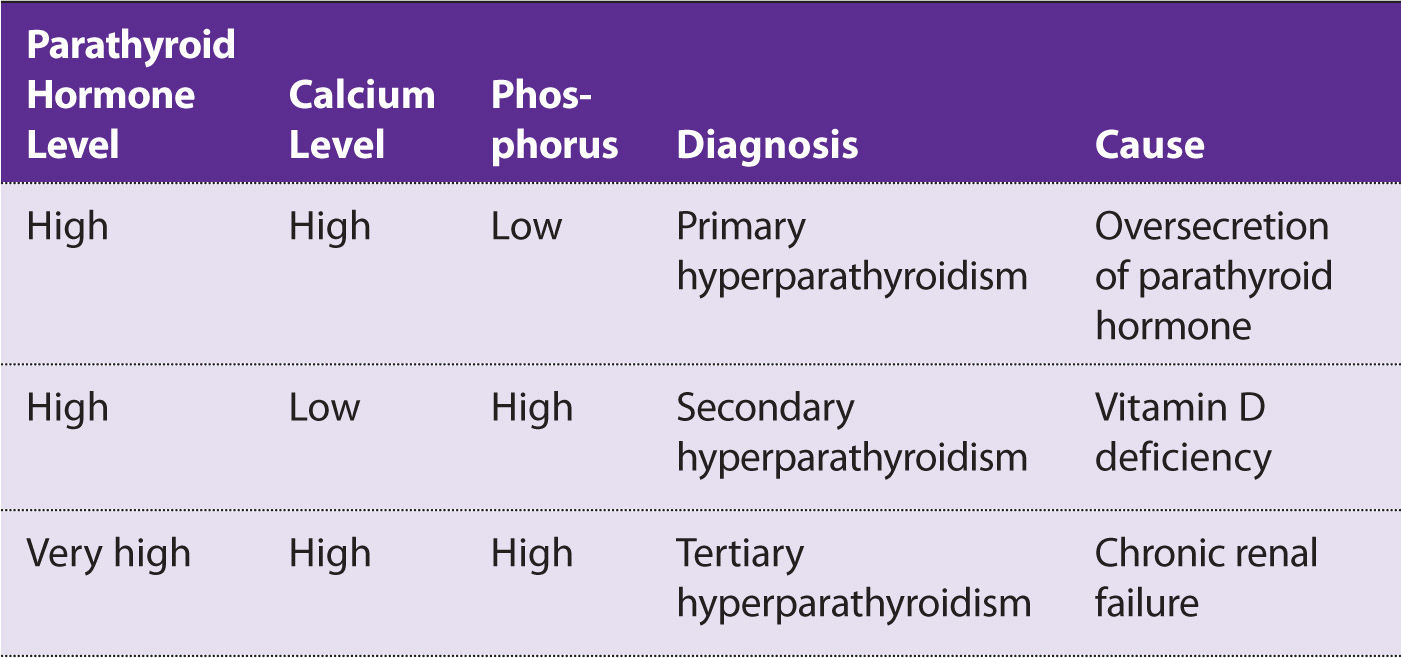
Primary hyperparathyroidism usually presents as asymptomatic hypercalcemia in a patient without renal disease. However, clinical signs that are subtle and suggest hypercalcemia in this patient outside of the elevation in the ion are normal vitamin D level, elevated PTH level, and normal albumin level. PUD may be caused by calcium being the second messenger for gastrin, causing an elevation of HCl release from parietal cells. Secondary hyperparathyroidism is from low calcium. This increases PTH from loss of negative feedback. Secondary hyperthyroidism can be caused by vitamin D deficiency causing low serum calcium levels. Tertiary hyperparathyroidism is seen in patients with long-standing secondary hyperparathyroidism, causing hyperplasia of the parathyroid glands. This is caused by chronic renal failure (Table 6-2).
Table 6-2 Differences in Serum Parathyroid Hormone, Calcium, and Phosphorus Levels in Primary, Secondary, and Tertiary Hyperparathyroidism
About 80% of patients with primary hyperparathyroidism will be asymptomatic. The remaining 20% present with “stones, bones, abdominal groans, and psychiatric moans.”
There are four parathyroid glands: right and left, and superior and inferior. The inferior glands are derived from the third pharyngeal pouch, and the superior are from the fourth pharyngeal pouch (Figure 6-2).
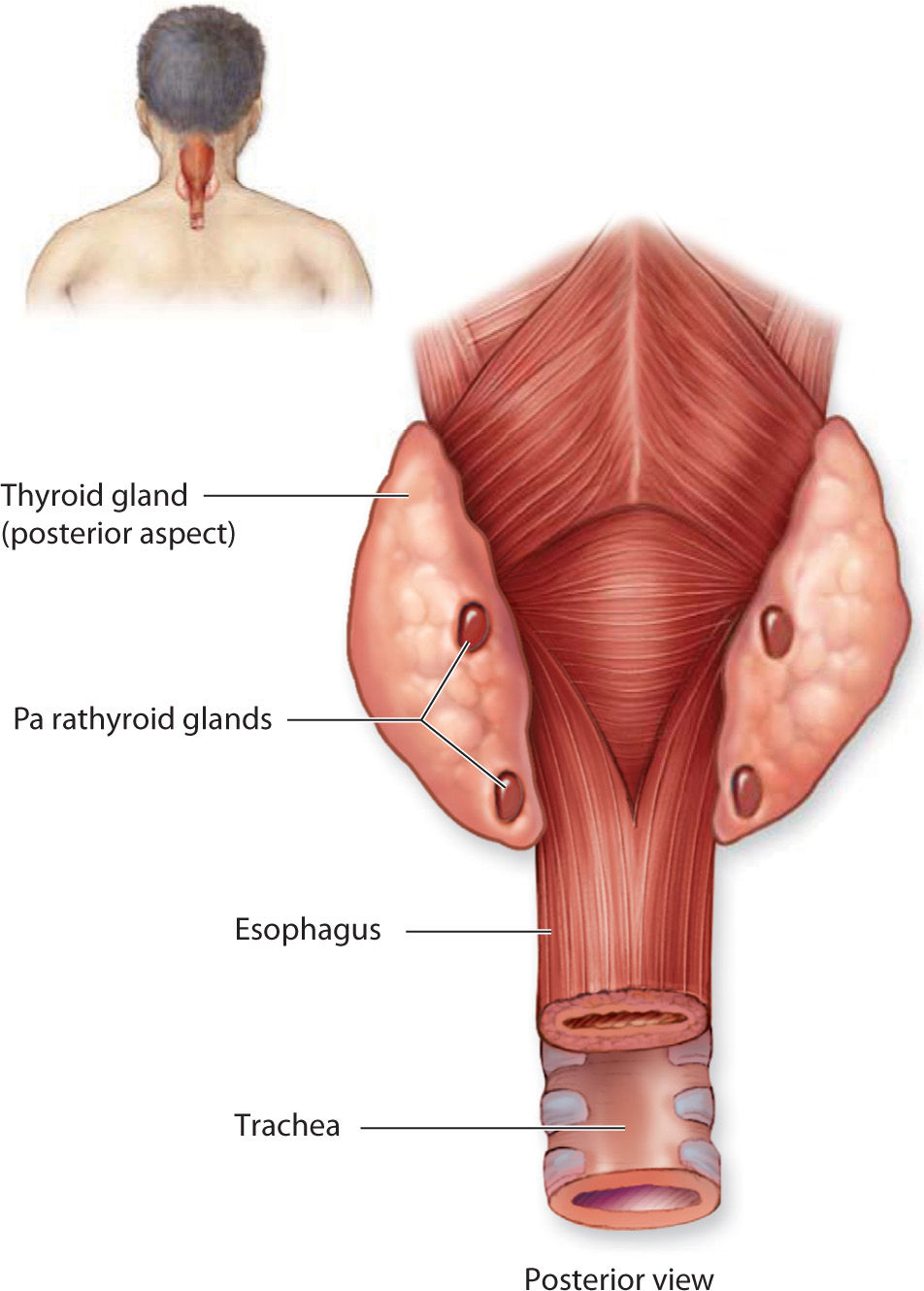
Figure 6-2. The parathyroid glands are four small nodules normally embedded in the capsule on the posterior surface of the thyroid gland. (Reproduced, with permission, from Mescher AL, ed. Junqueira’s Basic Histology: Text & Atlas. 13th ed. New York: McGraw-Hill; 2013.)
Multiple endocrine neoplasia (MEN) type I → 3 Ps
1. Pancreatic tumor (e.g., gastrinoma)
2. Pituitary adenoma
3. Parathyroid adenoma
Alkaline phosphatase levels are elevated in primary hyperparathyroidism.
What is the best next step in the management of this patient?
a. Thiazide therapy
b. Vitamin D supplementation
c. Surgical parathyroidectomy
d. Bisphosphonates
Answer c. Surgical parathyroidectomy
Surgical parathyroidectomy is indicated in patients with symptomatic hypercalcemia such as PUD, nephrolithiasis, abdominal pain, or altered mental status. Parathyroidectomy is the answer for asymptomatic patients with a serum calcium concentration of 1.0 mg/dL or above the upper limit of normal in those younger than 50 years of age, creatinine clearance reduced to less than 60 mL/min, and bone density with a T score less than –2.5. Thiazide therapy would make the calcium levels worsen and increase. Vitamin D supplementation is for patients with secondary hyperparathyroidism. Bisphosphonates are used in patients with concomitant osteoporosis.
Bisphosphonates inhibit osteoclastic bone resorption.
Thiazides cause hyperGLUC:
• HyperGlycemia
• HyperLipidemia
• HyperUricemia
• HyperCalcemia
Thiazides increase calcium uptake at the distal tubule.



