Chapter 29 Ear Disorders
The ear serves two functions—hearing and equilibrium. The ear includes both external and inner ear structures. Malfunctions of any of the ear structures can have impact on the ear itself as well as surrounding tissues. Additionally, ear dysfunction can cause systemic problems that have a lifelong impact. Adequate hearing is important for speech and language acquisition, academic performance, and socialization. Pediatric primary care providers must have an understanding of normal ear anatomy and physiology and be able to confidently identify, assess, and diagnose ear disorders in children. Deafness is discussed in Chapter 15.
 Development, Anatomy, and Physiology
Development, Anatomy, and Physiology
Anatomy and Physiology
The eustachian tube has three physiological functions with respect to the middle ear: (1) ventilation of the middle ear to equalize air pressure in the middle ear with atmospheric pressure and to replace oxygen that has been absorbed; (2) protection from nasopharyngeal sound, pressure, and secretions; and (3) drainage of secretions from the middle ear into the nasopharynx.
 Assessment
Assessment
History
The history of a patient with an ear disorder should include the following:
• Medical history significant for craniofacial abnormalities (e.g., cleft lip or palate) or syndromes associated with craniofacial anomalies (Down syndrome, Treacher Collins syndrome)
• Medical history pertinent to ear conditions (e.g., central nervous system infections, otitis media, trauma)
• Pain (onset, location, quality, duration, alleviating or aggravating factors)
• Associated symptoms, such as fever, vomiting and diarrhea, nasal congestion, or other symptoms of upper respiratory infection
• Exposure to risk factors: Environmental tobacco smoke (ETS), bottle propping, pacifier use, childcare, noise, swimming
• Family history of ear dysfunction
Physical Examination
The physical examination includes the following:
• Inspection of the external structures of the ear for symmetry, skin abnormalities, discharge, or lesions.
 The inner and outer canthi of the eye should form a straight line with the superior portion of the pinna. If the pinna inserts below this line, the ear is considered low-set, which can be associated with a number of genetic and congenital syndromes and renal issues.
The inner and outer canthi of the eye should form a straight line with the superior portion of the pinna. If the pinna inserts below this line, the ear is considered low-set, which can be associated with a number of genetic and congenital syndromes and renal issues.• Assessment of developmental milestones related to hearing and speech development (Box 29-1)
• Palpation and rotation of the external ear for tenderness and inflammation; push on the tragus and apply pressure to the mastoid process.
• Otoscopic examination, which is best accomplished in a young child at the end of the physical examination with the child on an examining table or seated on the parent’s lap. Pulling the ear downward, outward, and backward can enhance visualization of the EAC in infants and small children. In older children and adolescents, the EAC is lifted upward and backward, slightly away from the head.
• Decreased TM mobility secondary to effusion is noted through pneumatic otoscopy, tympanometry, or acoustic reflectometry.
• Examine the canal for redness, edema, or discharge. Assess all 360 degrees of the TM, the bony processes, and the cone of light (see Color Plate). Look for air-fluid level or bubbles behind the TM. Note any retraction, perforation, redness or other alteration in color, fibrosis, bulging, or retraction.
BOX 29-1 Developmental Milestones Used to Assess Hearing
12 to 18 Months
Points to unexpected sound or familiar objects when asked
Follows simple direction without cues
Data from Northern J, Downs M: Hearing in children, ed 4, Baltimore, 1991, Williams & Wilkins.
Common Diagnostic Studies
• Evoked otoacoustic emission (EOAE) testing is the method of hearing screening used for universal newborn screening. Dr. David Kemp first described the phenomenon of otoacoustic emissions in 1978. He found that the normal-hearing ear has the ability to emit detectable sounds called spontaneous otoacoustic emissions. The normal ear also emits these sounds when given a stimulus (EOAE) and provides evidence that the outer hair cells of the cochlea are functioning appropriately and hearing is likely to be intact. EOAE is efficient, highly sensitive, and easy to perform in a quiet, cooperative child, which makes it conducive for use in newborns. However, the EOAE does not quantify hearing deficit and may not identify auditory nerve dysfunction; ambient room noise and an uncooperative child may interfere with the test and provide unreliable results. Improvements in EOAE and auditory brainstem response technology have resulted in highly acceptable levels of hearing sensitivity and specificity at relatively low cost (Nelson et al, 2008).
• Auditory brainstem response (ABR) measures the initiation of sound-induced electrical signals in the cochlea. The ABR measures the functioning of the peripheral auditory system and neurological pathways related to hearing. Although it is not a direct measure of hearing, ABR allows for inferences to be made about hearing thresholds. The ABR is useful in identifying hearing loss in a young infant or in children unable to cooperate with EOAE or audiometry. Occasionally sedation is required. Neurological abnormalities may make interpretation of an ABR impossible. Automated ABR is available as a screening device.
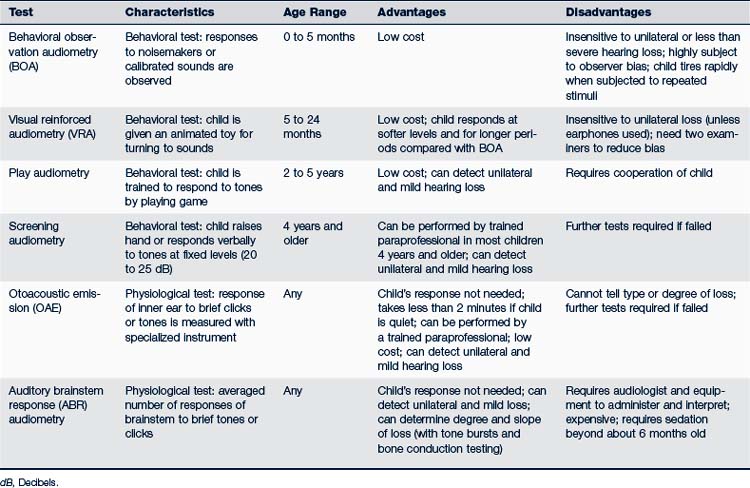
• Audiometry, useful in assessing hearing loss in older children, measures hearing threshold via bone or air conduction, or both, in decibels at varying frequencies (Tables 29-1 and 29-2). Twenty dB is about as loud as a whisper, 40 dB is normal speaking loudness, and 90 dB produces pain. The frequencies of normal speaking range from 250 to 4000 Hz. Hearing loss, especially in the higher frequencies (2000 to 6000 Hz), can cause significant problems in understanding speech. A screening audiogram that tests each ear at 20 dB and frequencies of 500, 1000, 2000, and 4000 Hz is a useful assessment tool in office pediatrics. If a more detailed audiogram is needed, a qualified audiologist should perform it.
• Pneumatic otoscopy helps assess TM mobility. A good seal with the speculum and otoscope is required before insufflation of air into the ear canal. Brisk movement of the membrane should be seen; altered mobility suggests MEE or possible perforation.
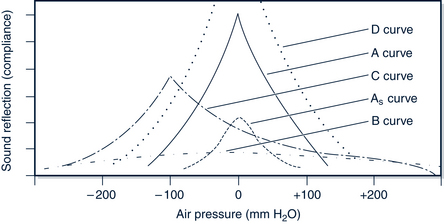
• Tympanometry evaluates the function of the middle ear by assessing the movement of the TM by applying from −400 to +100 mm H2O pressure to the ear canal. Movement of the TM is translated into a graph called a tympanogram (Fig. 29-1). The type A tympanogram has a compliance peak between ±100 mm H2O and reflects a normal TM. The type B tympanogram generally has no peak or a flattened wave and suggests effusion, perforation, or the presence of a pressure-equalizing tube (see Fig. 29-2). The type C tympanogram has a sharp peak between −100 and −200 mm H2O and reflects negative ear pressure (Fig. 29-2). Tympanograms are helpful when otitis media (OM) with effusion is persistent or a question remains regarding the results of physical examination of the eardrum. Tympanograms are of little use in children younger than 7 months old because their ear canals are hypercompliant in response to pressure from the tympanometer.
• Acoustic reflectometry is used to detect an MEE by directing a sound of varying frequency toward the TM and measuring the intensity of reflected sound. The reflectometer directs sounds of varying frequency toward the TM and measures the intensity of the reflected sound. The fluid-filled middle ear space restricts vibration of the eardrum, so sound is intensified when returning to the device. Unfortunately the reflectometer cannot distinguish if an MEE is serous or suppurative. Acoustic reflectometry is less accurate than pneumatic otoscopy.
• Tympanocentesis with aspiration of middle ear fluid is helpful for the relief of pain and identification of persistent infecting organisms. It is rarely used in clinical pediatrics and is generally considered outside the scope of practice of the primary care provider.
• Laboratory tests of blood and urine are rarely indicated unless questions remain regarding perinatal infection, systemic illness, or concomitant kidney dysfunction. Exudate from acute otitis media with perforation may be cultured.
• Genetic testing may be useful in determining if the hearing loss is inherited.
• Approximately 50% of all cases of congenital deafness are genetic. Of these 75% to 85% are inherited in an autosomal recessive pattern, 15% to 20% in an autosomal dominant pattern, and 1% X-linked (Moody and Strasnick, 2010).
TABLE 29-2 Evaluation of Audiometric Results
| Average Threshold at 500 to 2000 Hz (decibels) | Description | Significance |
|---|---|---|
| −10 to +15 | Normal | |
| 16 to 25 | Slight loss (minimal) | Difficulty hearing faint speech, slight verbal deficit |
| 26 to 40 | Mild loss | Auditory learning dysfunction, language, or speech problems |
| 41 to 55 | Moderate loss | Trouble hearing conversational speech, may miss 50% of class discussion |
| 56 to 70 | Moderately severe loss | |
| 71 to 90 | Severe loss | Educational retardation, learning disability, limited vocabulary |
| 90+ | Profound loss |
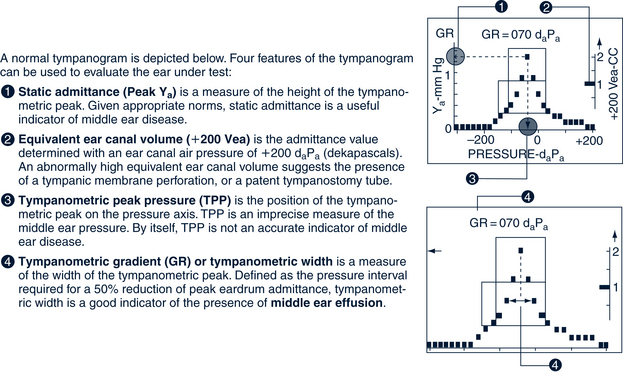
FIGURE 29-1 A normal tympanogram.
(From WelchAllyn: MicroTymp Portable Tympanometric Instrument operating instructions. Available at www.welchallyn.com, Skaneateles Falls, NY.)
 Management Strategies
Management Strategies
Removal of Cerumen
Cerumen in the ear canal can be removed mechanically, with the use of a ceruminolytic/softening agent, by gently irrigating the ear, or by a combination of these techniques (Roland et al, 2008; Shaikh et al, 2010). Before irrigation 2 or 3 drops of docusate sodium, mineral oil, or other warm oil may be instilled to help soften the obstructive wax. Baking soda mixed with water is also effective. Mix one-half teaspoon baking soda with 2 ounces of water and instill a few drops in the affected ear two times daily for 1 week. After 1 week the solution should be discarded. Tap-water irrigation alone is also as effective as using a softener before irrigation. For dry, hardened wax, softeners may decrease the amount of irrigant required. Irrigation is then accomplished by using a bulb syringe or “water jet” (on low setting). The irrigation solution can be warm water or hydrogen peroxide diluted 1:1 with warm water. Irrigation should not be attempted if the TM is possibly perforated or pressure-equalizing tubes (PETs) are in place. In a systematic review of the effectiveness of different cerumen removal methods, Clegg and colleagues (2010) found that sodium bicarbonate, olive oil, and water are more effective than no treatment. They also found that the effectiveness of irrigation versus mechanical cerumen removal was equivocal.
Follow-Up and Referral
An otolaryngology referral is indicated for unusual ear conditions, congenital malformation of the head and neck structures, craniofacial anomalies, sensory dysfunction involving hearing or speech, when appropriate therapy for OM has failed, or if ongoing effusion or infection persists. Myringotomy (and/or PET insertion) is indicated when there is severe, refractory pain; hyperpyrexia; facial paralysis, mastoiditis, labyrinthitis; or central nervous system infection; immunological compromise; and an ear infection that has failed two courses of antibiotics (Kershner, 2007). Referral to an audiologist is necessary if the ear pathology is prolonged or when the child’s ability to hear is questioned. Speech and language evaluations are imperative to resolve questions about whether the child’s verbal development is delayed because of persistent or recurring ear problems. Chapter 31 addresses criteria for tonsillectomy and adenoidectomy.
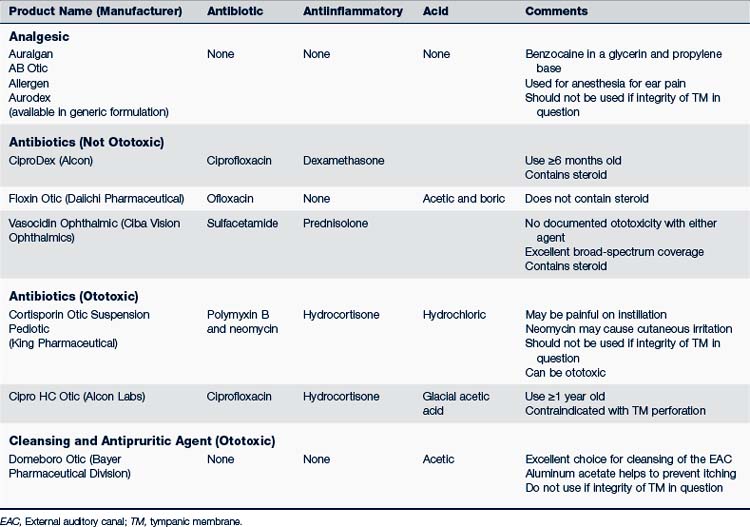
Pressure-Equalizing Tubes
Viral myringitis or early AOM without otorrhea in a child with PETs will most likely resolve spontaneously because of increased middle ear ventilation. Tympanostomy tube otorrhea (TTO) occurs usually when a child with PETs has an upper respiratory infection and has drainage coming from the tubes. TTO usually involves the same bacterial pathogens seen in AOM. Ototopical antibiotics are recommended because of their ability to concentrate the medication in the middle ear space; however, it is imperative that purulent material be removed from the canal prior to instilling the drops. Eardrops containing fluoroquinolone, with or without a corticosteroid, are the preferred treatment for TTO even in recurrent AOM (Granath et al, 2008; Schmelzle et al, 2008; Wall et al, 2009). Ototopical medications are listed in Table 29-3.
Many PETs fall out well before their usefulness has been expended. Once the PET has been extruded from the TM, follow-up every 6 to 12 months is suggested until the tube falls out of the external canal. For the rare set of PETs that remains in situ, surgical removal is suggested after 2 years. Complications of PETs include otorrhea, otitis externa (OE), granuloma, cholesteatoma, PET obstruction, persistent TM perforation, and tympanosclerosis. Bacterial biofilms can form on implanted prostheses, including PETs, and tend to be resistant to systemic antibiotics (Bakaletz, 2007).
Prevention of Noise-Induced Hearing Loss
Noise is a common cause of sensorineural hearing loss (SNHL) in children, and the pattern of damage depends on the frequency, intensity, and duration of the noise (Gifford et al, 2009). Any structure in the ear can be permanently damaged by noise greater than or equal to 140 dB. (See Chapter 41 for discussion of this environmental hazard and a list of risky noise sources.)
 Specific Ear Problems in Children
Specific Ear Problems in Children
Otitis Externa
Epidemiology
Furunculosis of the external canal is generally caused by S. aureus and Streptococcus pyogenes. Otomycosis is usually caused by Aspergillus or Candida and is caused by recent use of systemic or topical antibiotics or steroids. Otomycosis is also more common in children with diabetes or immune dysfunction, accounts for 10% of OE, and is most commonly caused by A. niger, Escherichia coli, Klebsiella pneumoniae, and group B streptococci are more common in neonates.
Clinical Findings
History
• Itching and irritation progressing to severe pain
• Pressure and fullness in ear and occasionally hearing loss that can be conductive or sensorineural
• Rare systemic complaints and symptoms
• Rare hearing loss and otorrhea
• Sagging of the superior canal, periauricular edema, and preauricular and postauricular lymphadenopathy with more severe disease. Extension to the surrounding soft tissue results in the obstruction of the canal with or without cellulitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree