6 Drowning
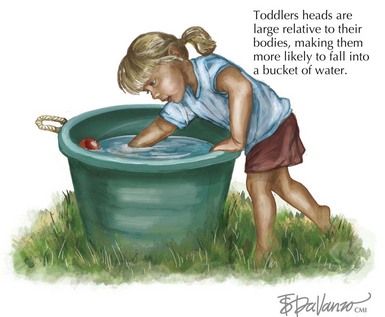
Pediatric drowning is the second leading cause of accidental childhood death in the United States, surpassed only by motor vehicle collisions. It is most common in young toddlers and adolescents, and boys are more likely to drown in all age groups. Toddlers are most likely to drown in small, household water sources such as bathtubs and buckets. Inadequate adult supervision is often responsible, although children have usually been out of sight for less than 5 minutes. Toddlers have large heads relative to their bodies, making them more likely to fall forward into buckets or tubs and less able to right themselves (Figure 6-1). Adolescents are more likely to drown during recreational activities such as boating and in natural bodies of water. Alcohol use contributes to up to 50% of teenage drownings. Pediatric drownings carry high morbidity and mortality; 30% to 50% of drowning victims die, and 10% survive with severe neurologic impairment.
Etiology and Pathogenesis
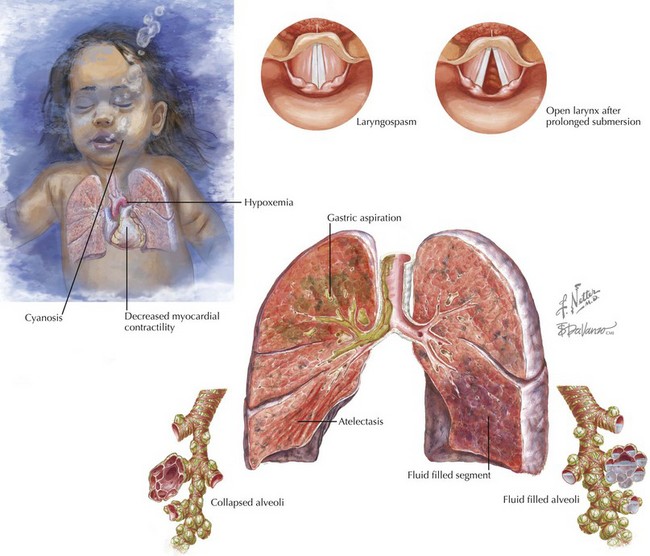
The effects of aspiration and continued submersion are many (Figure 6-2). Within the alveoli, water prevents diffusion of oxygen across the capillary/alveolar membrane. The capillary endothelium becomes increasingly permeable, resulting in pulmonary edema. Aspiration of gastric contents contributes to lung injury. As pulmonary edema and intrapulmonary shunt progress, hypoxia, hypercarbia, and acidosis ensue. These metabolic disturbances decrease myocardial contractility, increase systemic vascular resistance, and contribute to arrhythmias. If submersion continues long enough, drowning will progress to cardiac arrest. Clinically, there is little difference between fresh and salt-water drownings; however, there are some putative pathophysiologic differences. Whereas fresh water is particularly destructive to surfactant, salt water causes osmotic forces to draw additional fluid into the alveoli. Electrolyte disturbances are rare; however, ingestion of large amounts of fresh water can cause hyponatremia, and salt water ingestion can cause hypernatremia. Ingestion of large quantities of fresh water in the setting of hypoxemia may lead to hemolysis, although this is also a rare event.
Clinical Presentation
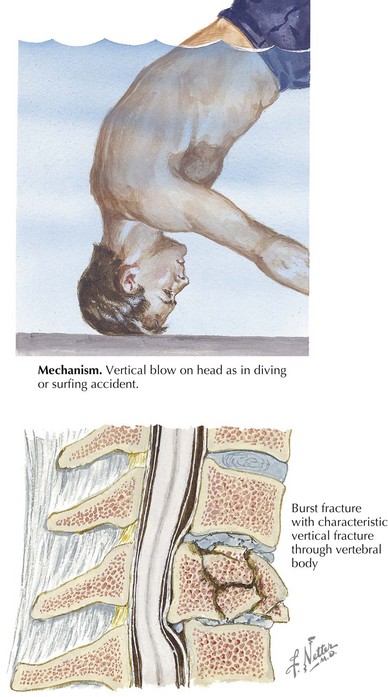
It is important to consider potential coexistent injuries and risk factors for drowning. Drowning may be associated with other trauma, including head injury, blunt abdominal trauma, and spinal injury (Figure 6-3). Seizures, cardiac arrhythmias, hypoglycemia, and intoxication can all contribute to a drowning event.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree