CHAPTER 5 smallest arteries in the circulatory system controlling the needs of organs and tissues. pressure reduction in a region of high flow speed. auscultatory sound within an artery produced by turbulent blood flow. noise in the Doppler signal caused by high-amplitude Doppler shifts. energy difference between two points. to move in a stream, continually changing position and direction. science or physical principles concerned with the study of blood circulation. the perceived color; any one or a combination of primary colors. the resistance to acceleration. consists of the arterioles, capillaries, and venules. positioning of multiple pulsed Doppler gates over the area of interest. maximum velocity at any given time. speed is constant across the vessel. predicts volume flow in a cylindrical vessel. difference in pressure required for flow to occur. a parameter used to convey the pulsatility of a time-varying waveform. predicts the onset of turbulent flow. electronic device that controls the region of Doppler flow detection. amount of blood moving in a forward direction; blood being ejected. the average velocity is calculated, with the colors placed side-to-side. rate of motion with respect to time. all measured velocities for each gate are averaged, then the colors are arranged up and down. the smallest veins that receive blood from the capillaries and drain into larger-caliber veins. the quantity of blood moving through the vessel per unit of time. • A difference in pressure (pressure gradient) is required for flow to occur. • Pressure difference can be generated by the heart or gravity. • Blood flows from the higher pressure to the lower pressure. • Equal pressure at both ends will result in no flow. • The greater the pressure difference, the greater the volume of blood flow. • Deoxygenated blood flows from the superior and inferior vena cava into the right atrium. • From the right atrium, blood courses through the tricuspid valve to the right ventricle. • Blood flows into the lungs through the pulmonary arteries from the right ventricle. • Oxygenated blood flows into the left atrium through the pulmonary veins. • Blood continues to flow through the mitral valve into the left ventricle. • From the left ventricle, blood is pumped into the aorta and systemic circulation. • Valves are present in the heart to permit forward flow and to prevent reverse flow. • Peripheral resistance is a primary regulatory control on cardiac output. • Vasodilation of the lower extremity arteries decreases resistance, increasing the flow to the limbs. • Vasoconstriction of the lower extremity arteries increases resistance, decreasing the flow to the limbs. • Malfunctioning valves can restrict forward flow (stenosis) or allow reverse flow by not closing completely (insufficiency or regurgitation). • Volume of blood passing a point per unit time. • Adult cardiac flows at a rate of 5000 mL/min. • Determined by the pressure difference and the resistance to flow. • Depends on the pressure difference, length and diameter of the tube, and viscosity of the fluid. • Cardiac Output = stroke volume × heart rate. • Stroke Volume (mL) = end diastolic volume minus end systolic volume. • Volumetric flow rate must be constant, because blood is neither created nor destroyed as it flows through a vessel. • The average flow speed in a stenosis must be greater than that proximal and distal to it so that the volumetric flow rate is constant throughout the vessel. • Blood flow is typically nonuniform through a specific vessel or throughout the body. • The muscular walls of the arterioles can constrict or relax, controlling blood flow to specific tissues and organs according to their needs. • Low-resistance waveforms demonstrate a slow upstroke in systole and a large amount of diastolic flow (i.e., internal carotid artery). • High-resistance waveforms demonstrate a sharp upstroke in systole and very little diastolic flow (i.e., external carotid artery). • Veins offer little resistance to flow. • Venous system demonstrates low-pressure, nonpulsatile flow. • Pressure is lowest when the patient is lying flat. • Greatest portion of the circulating blood is located in the venous system. • Veins accommodate larger changes in blood volume with little change in pressure.
Doppler instrumentation and hemodynamics
Hemodynamics
Cardiac circulation
CONTRIBUTING FACTORS
DESCRIPTION
Density
Mass per unit volume
Fluids
Substances that flow and conform to the shape of their containers
Gases and liquid
Kinetic energy
Proportional to its density and velocity squared
Mass
Measure of an object’s resistance to acceleration
Directly related to the inertia and force to accelerate
Pressure
Force per unit area
Driving force behind blood flow
Directly related to the blood flow volume
With each cardiac contraction, the blood is pressure-waved into the arteriole system and microcirculation
Equally distributed throughout a static fluid and is forced in all directions
Pressure gradient
Pressure difference required for flow to occur
Proportional to the flow rate
Resistance
The resistance of the arterioles accounts for about one half of the total resistance in the systemic system
The muscular walls of the arterioles can constrict or relax, producing dramatic changes in flow resistance
Directly related to the length of the vessel and fluid viscosity
Inversely related to the vessel radius
Velocity
Speed at which red blood cells (RBCs) travel in a vessel
Not constant or uniform across a vessel
Dependent on the left-ventricular output, resistance of the arterioles, cross-sectional area, and course of the vessel
Viscosity
A fluid’s ability to resist a change in shape or flow
Resistance to flow offered by a fluid in motion
Directly related to the number of RBCs
Blood is 4 times more viscous than water
Units—Poise or kg/m × s
Volumetric flow rate
Continuity rule
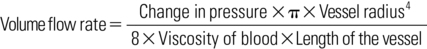
DEFINITION
RELATIONSHIP
Predicts flow volume in a long, straight cylindrical vessel
Directly related to the pressure difference and the size or radius of the vessel
Inversely related to the vessel length, resistance, and fluid viscosity
Relates to a steady flow in a long unobstructed tube
DEFINITION
RELATIONSHIP
Region of decreased pressure in an area of high flow speed
If flow speed increases, pressure energy decreases
Pressure decreases before a stenosis to allow the fluid to accelerate into the stenosis and decelerate out of it
Relates to short obstructed vessel
Types of blood flow
TYPE
DESCRIPTION
Laminar
Flow where layers of fluid slide over each other
Maximum flow velocity located in the center of the artery
Minimum flow velocity located near the arterial wall
Found in smaller arteries
Parabolic flow
Type of laminar flow
Average flow velocity is equal to one half the maximum flow speed at the center
Plug
Constant velocity across the vessel
Found in large arteries (i.e., aorta)
Pulsatile
Steady flow with acceleration and deceleration over the cardiac cycle
Includes added forward flow and/or flow reversal throughout the cardiac cycle in some locations in the circulatory system
Arterial diastolic flow shows the state of downstream arterioles
Disturbed
Altered or interrupted forward flow
Found at bifurcations and mild obstructions
Form of laminar flow
Turbulent
Random and chaotic flow pattern
Characterized by eddies and multiple flow velocities
Maintains a net forward flow
Onset predicted by a Reynolds number greater than 2000
Caused by a curve in a vessel’s course or a decrease in vessel diameter
Venous hemodynamics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Doppler instrumentation and hemodynamics
