54 Disorders of Thrombosis and Hemostasis
Etiology And Pathogenesis
Congenital Bleeding Disorders
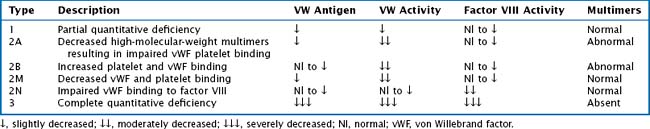
vWF is also a carrier protein for factor VIII; factor VIII unbound to vWF is rapidly degraded. vWD is classified into six types: 1, 2A, 2B, 2M, 2N, and 3. Table 54-1 provides a description and laboratory findings for all types of vWD.
Disseminated Intravascular Coagulation
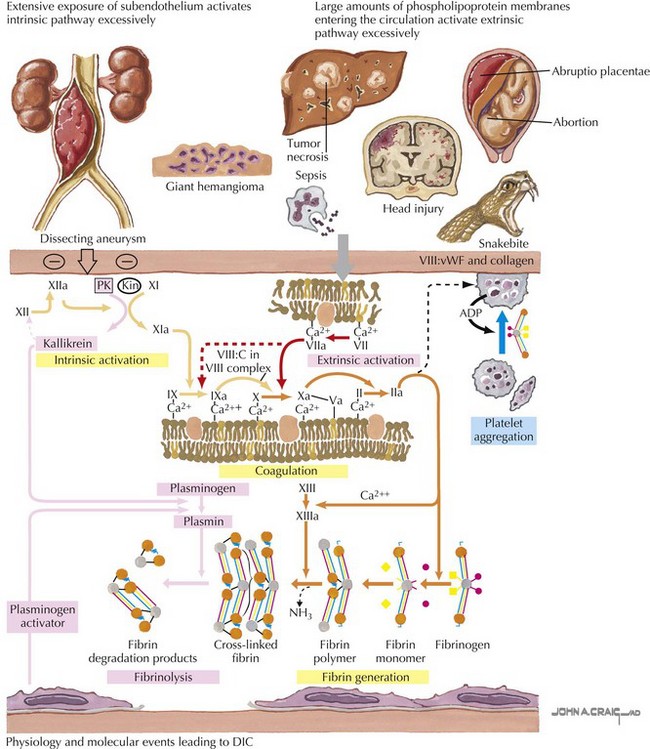
In disseminated intravascular coagulation (DIC), the normal physiology of coagulation is disturbed with resultant bleeding and thrombosis within the microvasculature. DIC is always secondary to a precipitating condition such as infection, tissue injury, malignancy, venom or toxin, or microangiopathic disorders. There is widespread deposition of intravascular fibrin leading to compromised organ function and capillary leak. Continued activation of this system leads to depletion of platelets and clotting factors, resulting in clinical bleeding (Figure 54-1).
Thrombosis
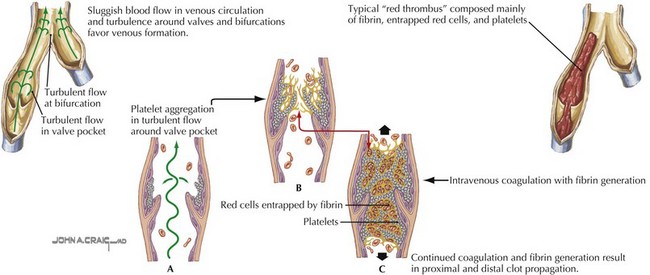
Deep venous thrombosis (DVT) is a consequence of Virchow’s triad of venous stasis, endothelial injury, and a hypercoagulable state. More than 90% of children with DVT have an identifiable prothrombotic risk factor. The most common risk factor is the presence of a central venous catheter (CVC). More than 50% of DVTs in children and more than 80% in neonates are associated with a CVC. Venous stasis in children may be caused by a postoperative state, casting or splinting, or other causes of prolonged immobility. Endothelial injury may be caused by trauma, infection, inflammation, or CVCs. Children may also have an inherited thrombophilia such as factor V Leiden or prothrombin gene mutations, deficiencies in the anticoagulant proteins including C, S, or antithrombin, hyperhomocysteinemia, or an elevated lipoprotein A. Acquired causes of thrombophilia include dehydration, antiphospholipid antibodies, malignancy, inflammatory states, anticoagulant deficiencies from consumption, or loss and exposure to certain medications such as estrogen-containing oral contraceptive pills or L-asparaginase (Figure 54-2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree