102 Disorders of the Respiratory System
Etiology and Pathogenesis
Several well-defined events are necessary for the transition to extrauterine life, including establishment of spontaneous respirations, clearance of amniotic fluid from the airway, surfactant release and function, and a decrease in pulmonary vascular resistance to aid in pulmonary blood flow. Impediments to one or more of these events generally manifest as respiratory distress in the newborn. The differential diagnosis of respiratory distress in neonates is broad, and nonrespiratory etiologies are varied (Table 102-1).
Table 102-1 Differential Diagnosis of Neonatal Respiratory Distress
| System | Category | Diagnoses |
|---|---|---|
| Respiratory | ||
| Cardiac | ||
| Neurologic | ||
| Metabolic |
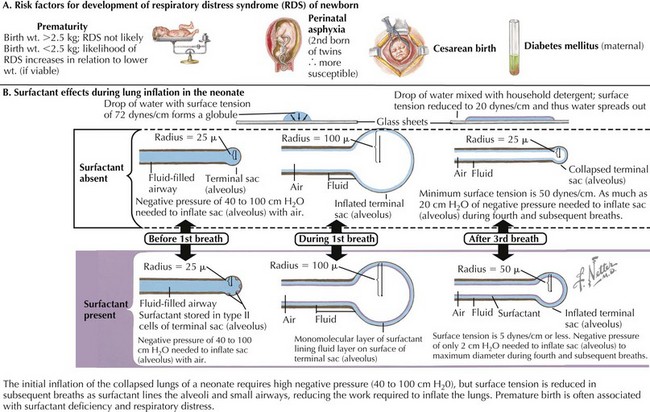
Respiratory Distress Syndrome
Respiratory distress syndrome (RDS), also known as hyaline membrane disease, is the end result of a relative surfactant deficiency that, when combined with the compliant chest wall of the neonate, promotes alveolar atelectasis and prevents newborns from developing a normal functional residual capacity (Figure 102-1). The most significant risk factor for RDS is prematurity because surfactant production begins between 24 and 28 weeks of gestation and does not become fully functional until at least 35 weeks. Other risk factors for the development of RDS include maternal diabetes; early-onset sepsis; and less commonly, congenital surfactant deficiency. Fifty percent of infants with birth weights between 500 and 1500 g develop some degree of respiratory distress; however, survival is greater than 90% with the use of exogenous surfactant and antenatal steroids.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree