32 Disorders of the Eye
Abnormal Red Light Reflex
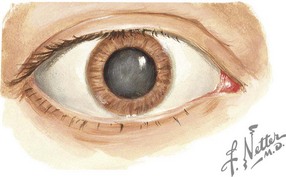
Cataracts
Congenital cataracts occur in two in 10,000 births (Figure 32-1). Of these, 20% to 25% of cases occur secondary to a congenital infection (rubella, cytomegalovirus, or toxoplasmosis) or as a component of a genetic or metabolic condition, such as Turner syndrome, Down syndrome, trisomy 13 and 18, galactosemia, and peroxisomal disorders. Children exposed to high-dose long-term corticosteroid therapy are also at risk, as are children with uveitis or who sustain ocular trauma.
Disorders of Eye Movement
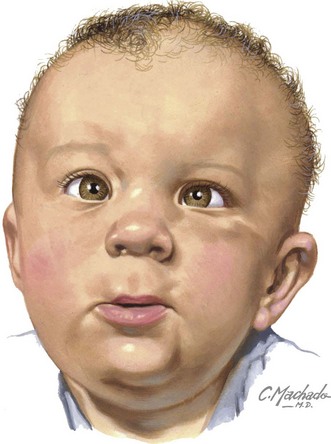
Strabismus
Misalignment of the eyes affects approximately 4% of children younger than 6 years of age (Figure 32-2). Heterophoria is the intermittent tendency for eyes to deviate, and heterotropia is a constant misalignment. The prefixes eso- (inward), exo- (outward), hyper- (upward), and hypo- (downward) indicate the direction of the misaligned eye. Other causes of eye deviations are cranial nerve palsies, intracranial or intraorbital mass, increased intracranial pressure (ICP), and myasthenia gravis.
Red Eye
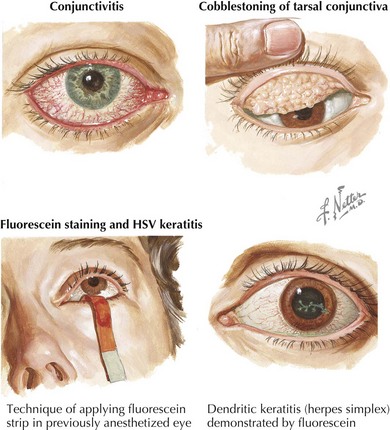
Viral Conjunctivitis
Viral conjunctivitis presents with watery or mucopurulent discharge, eye irritation, and scleral injection (Figure 32-3). Both eyes are usually affected simultaneously or in sequence. More serious infection causes pseudomembranes (inflammatory debris and fibrin) or true conjunctival membranes. Punctate keratitis and subepithelial opacities may also occur, causing decreased vision, photosensitivity, or glare and haloes around bright lights.
Other agents such as measles (rare because of widespread immunization), influenza, enterovirus, and herpes simplex virus (HSV) can cause conjunctivitis. Primary or recurrent HSV can also cause keratitis (corneal inflammation) with a dendrite pattern seen on fluorescein staining (see Figure 32-3). Treatment of ocular HSV includes topical antivirals (trifluridine, vidarabine, or iododeoxyuridine) and, depending on the extent of infection, oral or intravenous acyclovir. Consultation with an ophthalmologist is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree