Chapter 618 Disorders of the Conjunctiva
Conjunctivitis
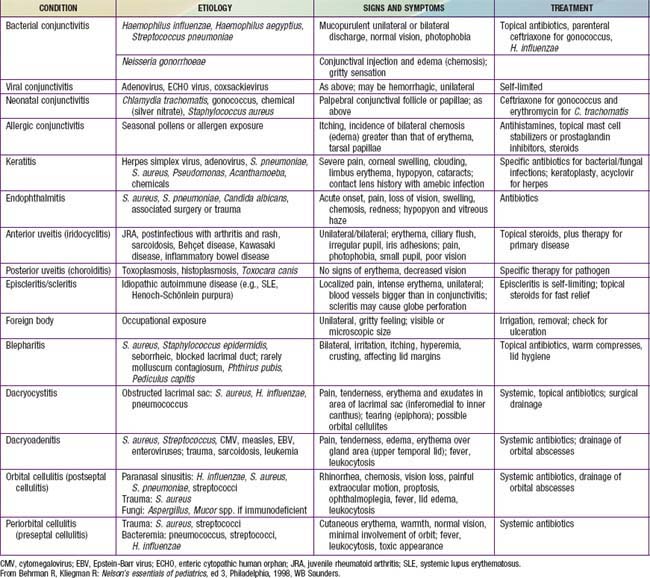
The conjunctiva reacts to a wide range of bacterial and viral agents, allergens, irritants, toxins, and systemic diseases. Conjunctivitis is common in childhood and may be infectious or noninfectious. The differential diagnosis of a red-appearing eye includes conjunctival as well as other ocular sites (Table 618-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree