73 Disorders of Growth
Etiology and Pathogenesis
Longitudinal Growth and Mediating Factors
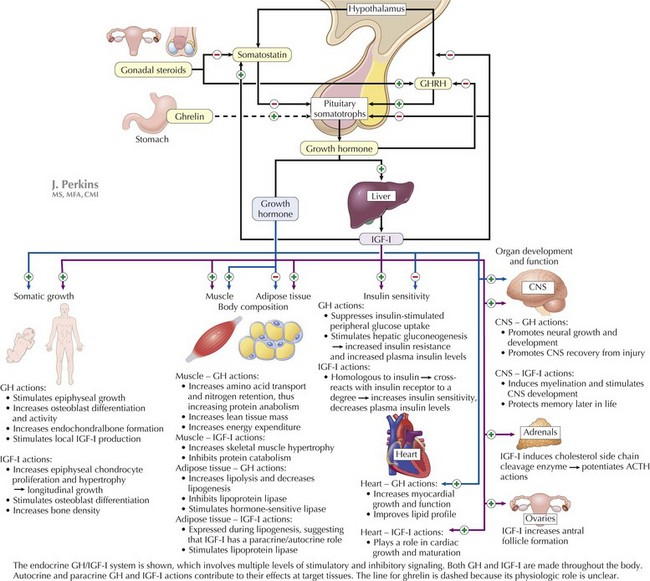
Growth hormone (GH) is the most important growth-regulating hormone; its pulsatile secretion from the anterior pituitary somatotrophs is regulated by two hypothalamic peptide hormones, GH-releasing hormone (GHRH) and somatostatin, which, respectively, stimulate and inhibit its release (Figure 73-1). Circulating GH is bound to GH-binding protein (GHBP), which corresponds to the extracellular domain of the GH receptor. Many, although not all, of GH’s actions are mediated through insulin-like growth factor (IGF)-I (i.e., somatomedin-C). Serum IGF-I is produced principally in the liver in response to GH and circulates in the bloodstream bound to IGF-binding proteins (especially IGFBP-3) that control its bioavailability. IGF-I acts at target tissues by binding cell-surface IGF receptors and triggering multiple downstream effects that include cellular hypertrophy and proliferation. IGF-I and free fatty acids also inhibit GH secretion at the level of the pituitary and hypothalamus.
Clinical Presentation
The causes of short stature can be divided into three general categories: chronic disease (including undernutrition), familial short stature (FSS), and constitutional delay of growth and puberty (CDGP) (Figure 73-2). Endocrine diseases are rare causes of short stature and are distinguished from other causes of short stature by linear growth failure that is more significant than weight loss. In developed countries, most short children have FSS, constitutional growth delay, or both. Short stature and constitutional growth delay are diagnoses of exclusion. The following is a focused review of the clinical presentations of selected normal variants and causes of short stature; see Box 73-1 for a comprehensive list of growth disorders.
Box 73-1 Differential Diagnosis of Short Stature
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree