Chapter 10 Diseases of the Cervix
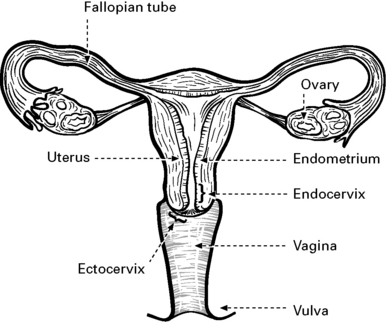
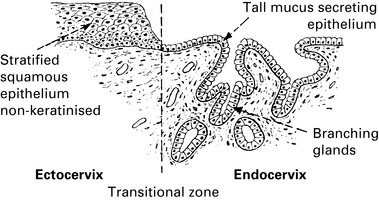
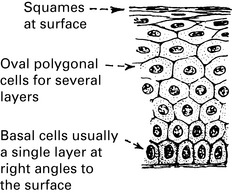
Normal cervical epithelium
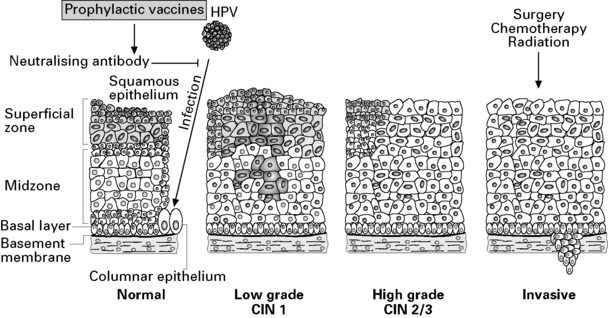
The role of human papilloma virus in cervical disease
Screening for cervical cancer
Screening process
The Cervical Smear
In Scotland, the current cervical screening programme includes the following:
– A national electronic database records and monitors the cervical smear process from the point of invitation to the completion of a colposcopic assessment. This is the Scottish Cervical Call-Recall System (SCCRS).
An abnormal smear is usually an indication for colposcopy (see p. 179).
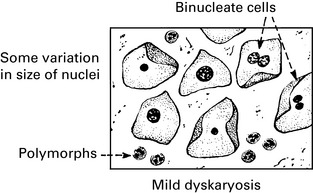
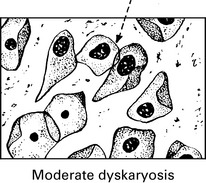
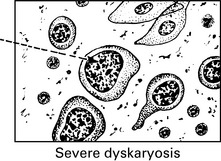
Cervical Smears
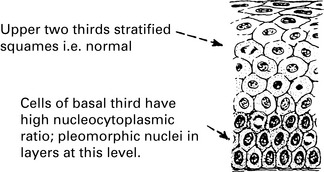
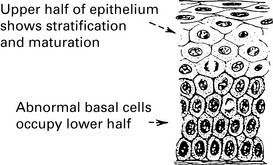
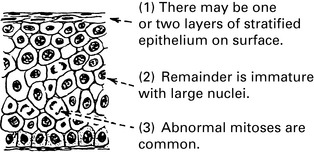
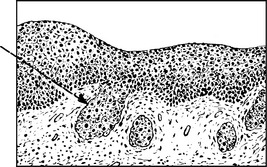
Premalignant and malignant cervical disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree