Nausea and retching are common in the early weeks of pregnancy, sufficiently so almost to be recognised as evidence of being pregnant. Although often described as morning sickness, symptoms can occur at any time of the day. Most women cope with this readily and the problem disappears spontaneously by the end of the first trimester. Sometimes, however, drug treatment may be necessary and antihistamines such as cyclizine or a phenothiazine can be prescribed safely.
HYPEREMESIS GRAVIDARUM
TREATMENT OF HYPEREMESIS
RHESUS INCOMPATIBILITY
FISHER CLASSIFICATION OF RHESUS FACTOR
RHESUS INCOMPATIBILITY
ANTIBODY FORMATION AND DETECTION
Kleihauer Test
Coombs’ Test
EFFECTS ON FETUS AND NEONATE
Fetal Hydrops

Mild Haemolysis
Severe Haemolysis
Child
Pale
Golden yellow jaundice appears within minutes of birth
Liver
Slightly enlarged
Greatly enlarged
Spleen
Slightly enlarged
Much enlarged
Blood
Mild anaemia
Rapidly increasing anaemia
Hb 13–15 g per dl
Few reticulocytes
Numerous reticulocytes, erythroblasts, normoblasts, and early white cells
Bilirubin scarcely increased
Indirect & direct bilirubin increased and rising
Urine
Negative test for bile
Positive test for bile
PREVENTION OF RHESUS HAEMOLYTIC DISEASE
ROUTINE ANTENATAL PROPHYLAXIS
Prophylaxis after birth or a recognised sensitising event
MANAGEMENT OF PREGNANCY
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diseases of Pregnancy
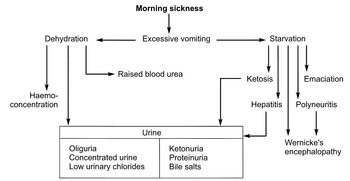
Occasionally there is a progression from ordinary nausea and vomiting to the rejection of all food and drink. Unchecked this may lead to dehydration and starvation with ketosis, liver damage, jaundice, neuropathies and even death.
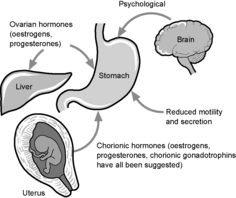
High levels of human chorionic gonadotrophin appear to elevate thyroxine levels and 60% of women with hyperemesis have biochemical or clinical hyperthyroidism.
1. Admit to hospital.
2. Exclude other causes of vomiting such as urinary tract infection and surgical causes such as appendicitis and bowel obstruction.
3. Blood taken for haemoglobin, urea & electrolytes, glucose, liver function tests, thyroxine and TSH levels.
4. Restrict oral intake initially.
5. Intravenous fluids should be given to treat any dehydration.
6. Prepared feeds via a fine naso-gastric tube are usually effective, the volume being given ideally through a pump system delivering small volumes over time. The volume given can progressively be increased.
7. Gradual reintroduction of oral foods.
8. Pyridoxine, 25 mg three times daily by mouth, may be effective in severe nausea.
9. Low-dose intravenous infusions of promethazine have been found useful in some centres.
10. Rarely, total parenteral nutrition or even termination of pregnancy may be indicated.
In each individual Rhesus genes are carried on two chromosomes, either of which may be handed on to the succeeding generation. There are six main Rhesus genes, three carried on each chromosome. Of the six, three are dominant C, D and E and three, their alleles, c, d, e are recessive. Each chromosome has a C locus, a D locus and an E locus which may be occupied by a dominant or recessive gene of the particular type.
The most important gene in Rhesus incompatibility is the dominant D gene. Because of this people possessing the D antigen are commonly described as Rhesus positive. When it is absent from both chromosomes its place is occupied by the recessive allele and the individual is termed Rhesus negative. Formerly more than 95% of cases of Rhesus disease were due to anti-D antibodies. With the introduction of anti-D prophylaxis (see page 109), however, the incidence of the disease due to this antibody has fallen sharply and haemolytic disease due to Rhesus antibodies other than D, anti-c and anti-E notably, is relatively more important. The term genotype means the mixture of genes on two chromosomes. For example:
CDe/cDE – Homozygous Rhesus (D) positive.
CDe/cde – Heterozygous Rhesus (D) positive.
cde/cde – Rhesus negative.
83% of the UK population are Rhesus positive, i.e. they possess at least one dominant D gene and of these 42% are homozygous and 58% heterozygous. This is of fundamental importance in pregnancy as all the offspring of a homozygous positive man will be Rhesus positive, while there is a 50% chance of a Rhesus negative child if the father is heterozygous positive and the mother Rhesus negative.
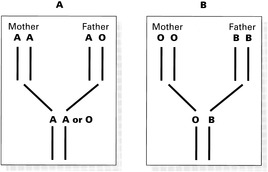
The circumstances might be as follows.
In family A the fetal blood is compatible with maternal group and fetal cells will continue to circulate in the maternal circulation. If the mother is Rhesus negative and the fetus is Rhesus positive then antibodies will form. The fetal cells in example B are incompatible with the maternal blood and will be rapidly destroyed on entering the maternal circulation. No antibodies are likely to form even if there is Rhesus incompatibility.
Before Rhesus immunisation is likely to occur the red cells of the fetus must have a blood group either the same as the mother or group O, and must possess a Rhesus gene not found in the mother.
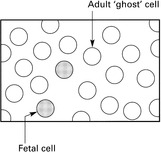
The presence of fetal cells in the mother’s circulation can be demonstrated by this test. It depends on the fact that fetal haemoglobin is more resistant than adult to acid elution. When a blood film is stained following elution the fetal cells will stand out against the adult ‘ghost’ cells. It is roughly quantitative by counting the number of fetal cells per 50 low power fields. Five cells per 50 fields = a bleed of 0.5 ml.
This test depends on the fact that antibodies are globulins. If these globulins are injected into an animal antibodies to them will be formed. These antibodies can in turn be used to detect the presence of the original antibodies. The Coombs’ reagent therefore is immune anti-globulin.
The DIRECT test is used to detect an affected fetus at birth. Cells from cord blood are suspended with the reagent and if the baby is affected (has maternal antibody attached) agglutination will occur.
The INDIRECT test (IAGT) is used to detect and measure antibody in the mother’s serum. This is suspended with test cells. Antibody in the serum will coat the cells and agglutination will occur when the Coombs’ reagent is added. By using dilutions of the mother’s serum a measure of the amount of antibody (titre) is obtained.
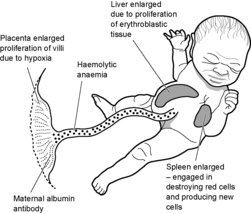
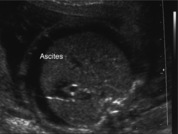
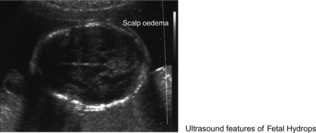
In its most severe form the process produces Fetal Hydrops which is fatal either in utero or after birth unless it can be detected at an early stage in utero and treated by direct transfusion. Here the severity of the anaemia has resulted in cardiac failure with widespread oedema, ascites and pleural effusions. The diagnosis may be made in utero by ultrasound.
In less severe degrees of the condition the baby may be born alive and quickly becomes jaundiced. Treatment by exchange transfusion (see page 112) may be needed. In the least affected babies jaundice does not occur but the child becomes progressively anaemic and may require top-up transfusion.
Kernicterus is a condition which may arise in any form of neonatal jaundice when the unconjugated bilirubin level rises above 340 micromoles/l. Rhesus incompatibility is the main cause. Bilirubin enters the fetal brain tissue, causing necrosis of neurones especially in the basal ganglia. The infant becomes lethargic and refuses to suck. Convulsions, rolling of eyes and head retraction develop. Death may occur. Physical and mental handicap usually follow if the baby survives.
If the fetus is Rh +ve these red cells will stimulate antibody formation. The aim is to ‘hide’ the D antigen so that the maternal immune mechanism does not recognise the cells as ‘foreign’ and antibodies will not then be formed. This is done by giving the mother anti-D which attaches itself to the D antigens of the fetal red cells making them unrecognisable by the immune mechanism and therefore incapable of stimulating antibody formation.
Around one per cent of pregnancies in Rhesus negative women will result in immunisation of the mother even in the absence of an identified event such as antepartum haemorrhage. As a result routine prophylaxis of these women is given in the form of Anti-D given routinely at 28 and 34 weeks gestation.
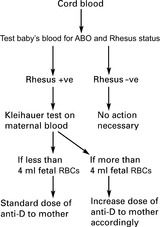
Tests are carried out as in the flow diagram.
All Rhesus negative women, without antibodies on re-testing, giving birth to Rhesus positive babies, are given an injection of anti-D immunoglobulin. This is done even if the Kleihauer test is negative. The standard dose is 500 i.u. by intra-muscular injection within 72 hours of delivery.
A rough estimate of the amount of fetal blood escaping into the mother’s circulation is made by the Kleihauer test and the dose of anti-D may be adjusted accordingly.
Where the pregnancy ends before 20 weeks the blood group of the fetus will not usually be known and 250 i.u. of anti-D should be given.
Similarly, when invasive procedures such as amniocentesis or external version are carried out anti-D is given. Other episodes of placental separation such as threatened miscarriage and antepartum haemorrhage should be covered by anti-D administration, the dosage being determined by the stage of pregnancy and the estimated volume of the bleed.
