Chapter 4 Diathermy and lasers
Diathermy
Diathermy has been used in surgical procedures for over 100 years (d’Arsonval 1893) for cutting and coagulation of tissues. Harvey Cushing pioneered the use of electrosurgery in neurosurgery, using a generator designed by Bovie in the 1920s, and this name is still synonymous with diathermy to some surgeons.
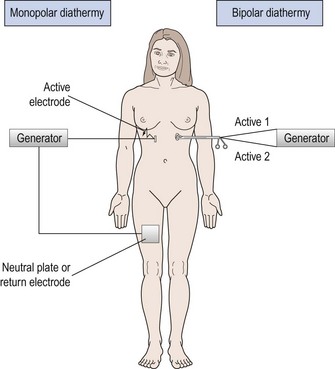
Monopolar diathermy
In monopolar diathermy, one electrode is applied to the patient who becomes part of the circuit. The surface area of the electrode plate is much greater than the contact area of the diathermy instrument to ensure that heating effects are confined to the end of the active electrode (Figure 4.1). The advantage of monopolar diathermy is that it can be used to cut as well as to coagulate tissues.
Tissue effects of diathermy
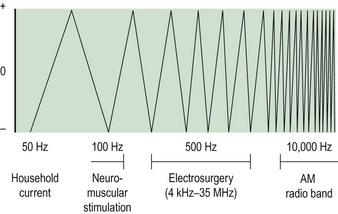
When household electrical current of 50 Hz frequency passes through the body, it causes an irreversible depolarization of cell membranes. If the current is sufficiently large, depolarization of cardiac muscles will occur and death may result. If household current is modified to a higher frequency, above 200 Hz, depolarization does not occur; instead, ions are excited to produce a thermal effect. This is the basis of diathermy. Figure 4.2 illustrates how the frequency of a current influences the effects on the body.
Factors which influence the effect of diathermy
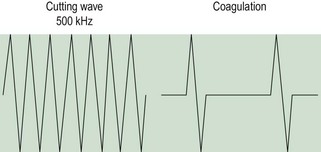
Cutting and coagulation
When the electrode is brought into direct contact with tissue and the waveform is modulated, coagulation occurs rather than vaporization. An intermittent waveform is used and thus bursts of thermal energy are interspersed with periods of no energy (Figure 4.3). For the power delivered to the tissue to remain constant, the electrosurgical unit must deliver a higher voltage to compensate for the episodes when no energy is delivered (up to 90% of the time with pure coagulation current). Thus, whilst cutting current at 50 W power will produce a high-frequency current of approximately 200–1000 V, a coagulation current may produce over 3000 V to deliver the same wattage to the tissue. The coagulating effect is produced by slower desiccation and shrinkage of adjacent tissue, producing haemostasis. The higher voltage produced by coagulation current carries a higher risk of inadvertent discharge of energy.
Duration of application
The longer the duration of application of electrosurgical current, the greater the extent of thermal injury. Research on uterine tissue shows that the duration of exposure of the tissue to current, rather than the wattage used, was the most important factor in producing tissue damage (Duffy et al 1991).
Heat and tissue injury
Diathermy current produces thermal injury to tissues. The temperature generated will dictate the degree of injury (Table 4.1). If carbon is seen on the tip of the diathermy electrode, the surgeon can assume that, at some stage, a temperature of 200°C has been reached.
Table 4.1 The degree of injury caused at different temperatures
| Temperature (°C) | Tissue effect |
|---|---|
| 44 | Necrosis |
| 70 | Coagulation |
| 90 | Desiccation |
| 200 | Carbonization |
Short-wave diathermy
Electrode redesign has led to an interest in the use of short-wave diathermy for its tissue destructive effect (Phipps et al 1990). It has been used in endometrial ablation. In this, the two electrodes form a capacitor in the output circuit with the patient providing the dielectric medium between the two plates. Frequencies of approximately 27 MHz are employed with power levels of approximately 500 W. By altering the shape and size of the electrodes, heating effects may be localized or diffused as required. However, care must be exercised as the effects are not always predictable.