111 Diarrhea
Pathophysiology
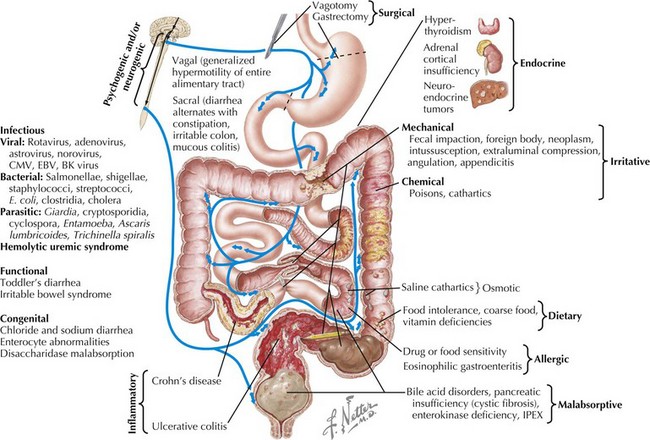
A total of 8 to 9 L of fluid enters the healthy intestines on a daily basis. Only 1 to 2 L are derived from food and liquid intake; the rest is from salivary, gastric, pancreatic, biliary, and intestinal secretions. Each day, about 90% of this fluid is absorbed in the small intestine, 1 L enters the colon, and about 100 mL is excreted in stool. Normal stool output is approximately 100 to 200 g/d. Diarrhea is defined as stool output greater than 200 g/d in children older than 2 years of age and greater than 10 mL/kg/d in children younger than 2 years of age. It is also described more practically as an increase in liquidity and frequency of bowel movements. Diarrhea can be categorized by duration, as either acute (≤2 weeks) or chronic (>2 weeks), or by mechanism, as osmotic or secretory. It can also be categorized by the presence or absence of malabsorption (Figure 111-1).
Acute Diarrhea
Etiology And Pathogenesis
The most common cause of acute diarrhea is infection (see Chapter 96). In young children, this is most often viral, with the most common agents being rotavirus, adenovirus, astrovirus, and norovirus. Norovirus causes 60% to 90% of nonbacterial gastroenteritis in the United States, affecting 23 million Americans each year. Rotavirus is a leading cause of death in children younger than 5 years of age worldwide. In immunocompromised hosts, viruses, including cytomegalovirus, Epstein-Barr virus, and BK virus, should be considered. It is estimated that 70% of infectious diarrhea is foodborne, and thus a detailed history of exposures is very important (Table 111-1). Exposure to untreated water may cause giardiasis. Use of public swimming pools poses a risk of Shigella, Giardia, Cryptosporidium, and Entamoeba infection, with the last three being chlorine resistant. Home pets can transmit infections. For example, turtles carry Salmonella spp. History of foreign travel may narrow exposures based on the specific destination. The most common etiology of traveler’s diarrhea remains enterotoxigenic Escherichia coli. Cryptosporidium and Giardia spp. are responsible for most parasitic infections in developed countries. Cyclospora outbreaks have occurred in the United States. Clostridium difficile infection, previously thought to affect only hospitalized patients or those taking antibiotics, is now responsible for 40% of community-acquired diarrhea. A recent increase in C. difficile infections has been observed, some attributable to the resistant strain, BI/NAP1. An overgrowth of toxin-producing Clostridium organisms causes pseudomembranous colitis, which may be a potentially life-threatening condition. Vibrio cholerae remains a cause of illness and death in war zones and developing countries. The mechanism of infectious diarrhea is primarily secretory. It can quickly lead to electrolyte abnormalities and acidosis. Infection may result in villous atrophy, which can add an osmotic component. Mucosal healing after infection may lead to transient postinfectious diarrhea.
Table 111-1 Foodborne Infectious Agents
| Food | Associated Infectious Agent |
|---|---|
| Eggs | Salmonella |
| Dairy | Campylobacter jejunii |
| Vegetables | Clostridium perfringens |
| Pork | Clostridium perfringens Yersinia enterocolitica |
| Seafood | Aeromonas spp. Vibrio spp. Plesiomonas spp. |
| Rice | Bacillus cereus |
| Beef | Enterohemorrhagic Escherichia coli |
Several other causes of acute diarrhea, particularly in afebrile children, may be particularly concerning. Intussusception, a telescoping of two segments of bowel that occurs mostly in children between 6 months and 2 years of age, may present with bloody diarrhea (see Chapter 109). The typical presentation is colicky abdominal pain, vomiting, and an abdominal mass. “Currant jelly” stools do not occur in all patients with intussusception but are pathognomonic for the condition. Hemolytic-uremic syndrome (HUS) is an uncommon but potentially fatal illness that may present with acute bloody diarrhea. HUS begins as a mild gastroenteritis that evolves into hematochezia, microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure (see Chapter 64). Less commonly, appendicitis may present with abdominal pain and diarrhea as a result of colonic irritation from the inflamed appendix (see Chapter 5).
Other acute causes of diarrhea include inflammatory bowel disease (IBD; see Chapter 110), overfeeding (caused by increased osmotic loads), antibiotic-associated diarrhea (likely caused by changes in bowel flora), extraintestinal infections (otitis media, urinary tract infection, pneumonia), and toxic ingestions.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree