4 Diabetic Ketoacidosis
Diabetes is a chronic disease defined by hyperglycemia caused by insulin deficiency. (Chapter 71 provides a detailed discussion of diabetes mellitus.). This may be the result of a lack of insulin production, as in type 1 diabetes mellitus (T1DM) or the body’s ineffective use of the insulin it produces, as in type 2 diabetes mellitus. The most common form of diabetes in children is T1DM.
Etiology and Pathogenesis
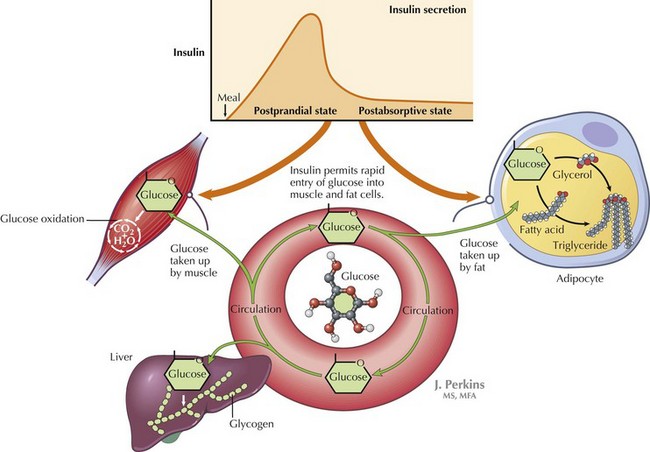
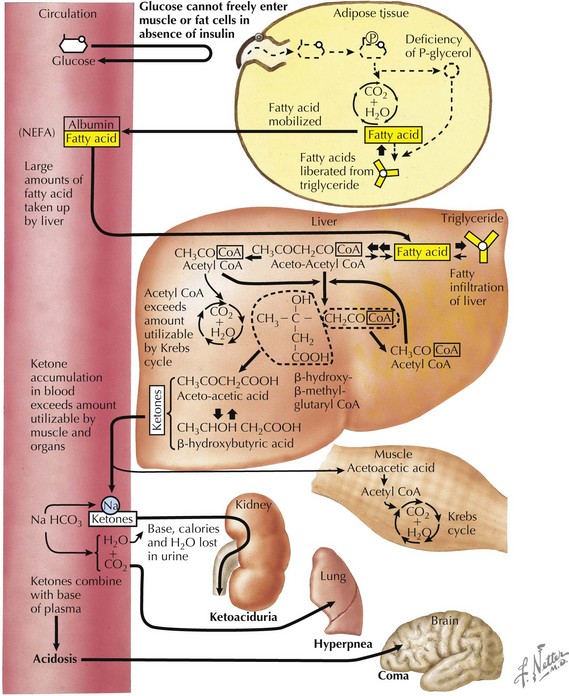
DKA is a result of insulin deficiency. Insulin is a hormone that responds to an increase in serum glucose via receptor-mediated utilization. This includes stimulation of glucose uptake from the blood by peripheral tissues; glycogen synthesis in the liver; and inhibition of processes that increase serum glucose, such as gluconeogenesis and glycogenolysis (Figure 4-1). In the absence of insulin, blood glucose levels increase. There is inability to store glucose that is absorbed through the gut, and because of the absence of insulin’s suppression of these pathways, production of new glucose via gluconeogenesis continues. This process is perpetuated by increased production of hormones that increase blood glucose, including glucagon, cortisol, and catecholamines. As blood glucose increases, osmotic diuresis occurs, resulting in urinary losses of electrolytes. Because the body cannot use the glucose that has been supplied, it responds as if in the fasting state. Fat is then broken down into free fatty acids to be used as fuel. Free fatty acids are converted to ketoacids, including β-hydroxybutyrate and acetoacetate, leading to metabolic acidosis (Figure 4-2).
Clinical Presentation
Patients with DKA typically present with acute symptoms of nausea and vomiting. In patients presenting with T1DM for the first time, there may be a history of polyuria, polydipsia, enuresis, or weight loss. As ketosis progresses, patients may become obtunded and unable to provide a history. Therefore, a glucose measurement should be obtained quickly in any patient who presents with altered mental status. (Hypoglycemia may also be manifested as altered mental status.) Ketosis may also result in presence of a fruity breath, which can help direct the diagnosis. On physical examination, patients generally show signs related to the degree of dehydration from chronic hyperglycemia and osmotic diuresis. This may include tachycardia, presence of dry mucous membranes, and delayed capillary refill. DKA should be suspected in patients with signs of dehydration who maintain a high urine output. Abdominal examination often reveals diffuse tenderness. It is important to document a detailed neurologic examination at presentation because patients who present with normal mental status may have an acute change in status with therapy. DKA leads to physical examination findings affecting many systems (Table 4-1).
Table 4-1 Physical Exam Findings in Diabetic Ketoacidosis
| Physical Examination Component | Findings | Interpretation |
|---|---|---|
| General | Can range from alert and interactive to obtunded based on the degree of dehydration and acidosis | Obtain a glucose measurement immediately on any patient presenting with altered mental status |
| HEENT | Dry mucous membranes, blurred vision, presence of fruity odor to breath | Ketosis tends to result in fruity odor to breath |
| Cardiovascular | Tachycardia | Indicative of dehydration |
| Lungs | Kussmaul respirations | Deep, sighing breaths used as respiratory compensation for metabolic acidosis Lungs are clear to auscultation, indicating the absence of an underlying lung pathology |
| Abdomen | Diffuse abdominal tenderness | Ileus may result from ketosis and can mislead the diagnosis toward an acute abdominal process |
| Extremities | Delayed capillary refill, decreased skin turgor | Indicative of dehydration |
| Intake and output | Increased | Indicative of thirst and increased fluid intake caused by osmotic diuresis |
HEENT, head, ears, eyes, nose, and throat.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree