71 Diabetes Mellitus
Diabetes mellitus includes a variety of conditions that share in common hyperglycemia caused by a deficiency of insulin action. Diabetes can occur as a result of autoimmune destruction of insulin-producing pancreatic β-cells that causes absolute insulin deficiency (type 1 diabetes), insulin resistance in peripheral tissues with relative insulin deficiency (type 2 diabetes), genetic mutations in β-cell function (monogenic diabetes of the young [MODY] and neonatal diabetes), and other causes (Box 71-1). Although type 2 diabetes accounts for 90% to 95% of diabetes in the United States, type 1 diabetes is the most frequent form in children, occurring in about one in 1500 children by age 5 years and one in 350 children by age 18 years. Over the past 20 years, however, as a result of the obesity epidemic, type 2 diabetes has been increasing in prevalence in the pediatric population. This chapter focuses on type 1 diabetes, with relevant comparisons to type 2 diabetes in children.
Box 71-1
Diabetes Mellitus Types
Adapted from American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care 34(suppl 1):62-69, 2011; and Botero D, Wolfsdorf JI: Diabetes mellitus in children and adolescents. Arch Med Res 2005;36:281-290.
Etiology and Pathogenesis
Type 1 Diabetes Mellitus
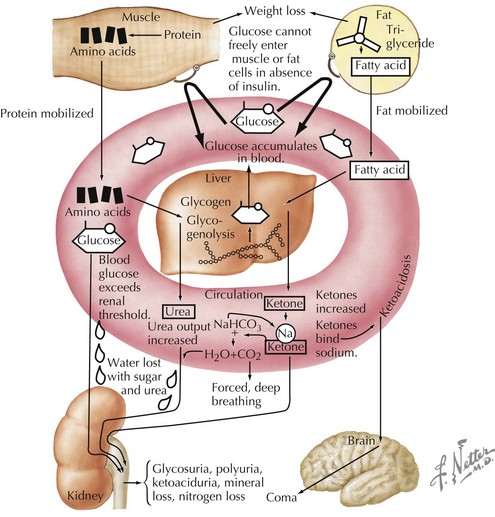
Insulin is an anabolic hormone that stimulates glucose uptake and hepatic glycogen synthesis and inhibits hepatic gluconeogenesis and glycogenolysis. It also stimulates lipogenesis, amino acid uptake, and protein synthesis (see Chapter 4, Figure 4-1). The absence of insulin triggers a series of biochemical events that emulate a starvation state even when food intake is adequate and that result in hyperglycemia and ketoacidosis (Figures 71-1 and 4-2). Glucose uptake by peripheral tissues is reduced, and hepatic glycogenolysis and gluconeogenesis are stimulated by insulin deficiency, which produces hyperglycemia. Lipolysis, proteolysis, and fatty acid oxidation lead to the accumulation of ketone bodies (β-hydroxybutyrate and acetoacetate), which eventually leads to metabolic acidosis.
As the serum glucose increases above 180 mg/dL, the renal threshold for glucose reabsorption, glycosuria results. Glycosuria causes an osmotic diuresis, resulting in polyuria and compensatory polydipsia. Over time, hyperosmolarity and dehydration develop, and decreased tissue perfusion can elicit a mild lactic acidosis. Patients without free access to fluid, such as infants and those with developmental disorders, are especially at risk. The osmotic diuresis also leads to the loss of crucial electrolytes, such as sodium, potassium, phosphorus, magnesium, and calcium. Metabolic acidosis and dehydration also stimulate counterregulatory hormones, such as growth hormone, cortisol, and epinephrine, further antagonizing insulin action. The end result is a serious metabolic disorder termed diabetic ketoacidosis (DKA; see Chapter 4).
Clinical Presentation
Complicating the presentation is the fact that patients with new-onset diabetes often present during an intercurrent illness, which may confound the classic presentation of diabetes. In addition, a number of other conditions should be considered in the differential diagnosis of diabetes (Table 71-1).
Table 71-1 Differential Diagnosis
| Symptom | Differential Diagnosis |
|---|---|
| Polyuria | Diabetes insipidus, urinary tract infection, psychogenic polydipsia |
| Polydipsia | Diabetes insipidus, psychogenic polydipsia |
| Glycosuria | Benign renal glycosuria |
| Weight loss | Anorexia nervosa, inflammatory bowel disease, celiac disease, infectious disease |
| Vomiting, abdominal pain | Gastroenteritis, inflammatory bowel disease, appendicitis, toxic ingestion, pancreatitis |
| Abnormal breathing | Pneumonia, asthma exacerbation |
| Hyperglycemia | Stress-induced hyperglycemia, medication-induced hyperglycemia |
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree