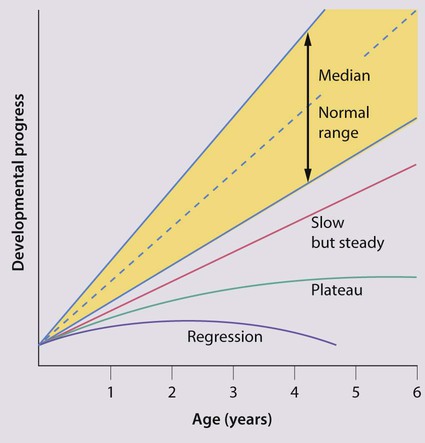
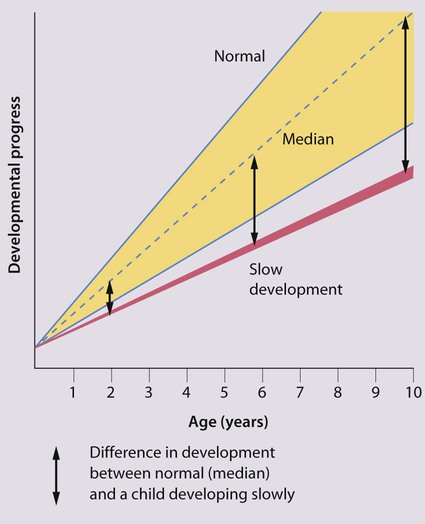
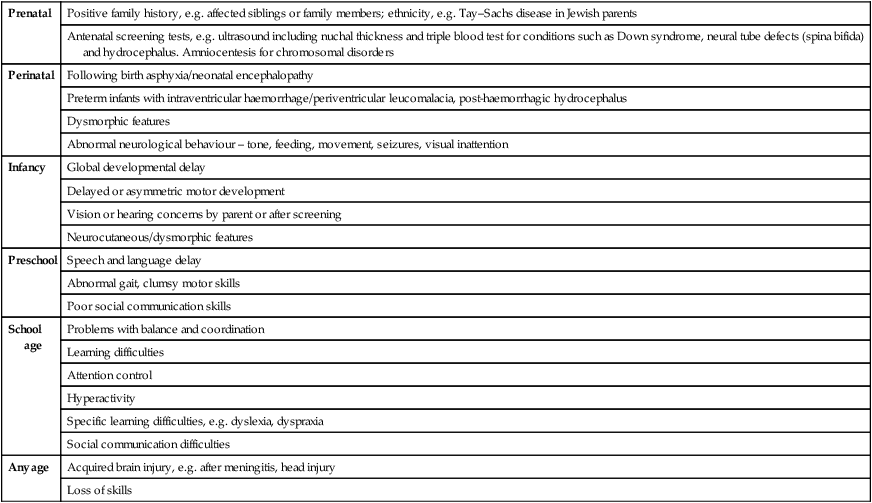
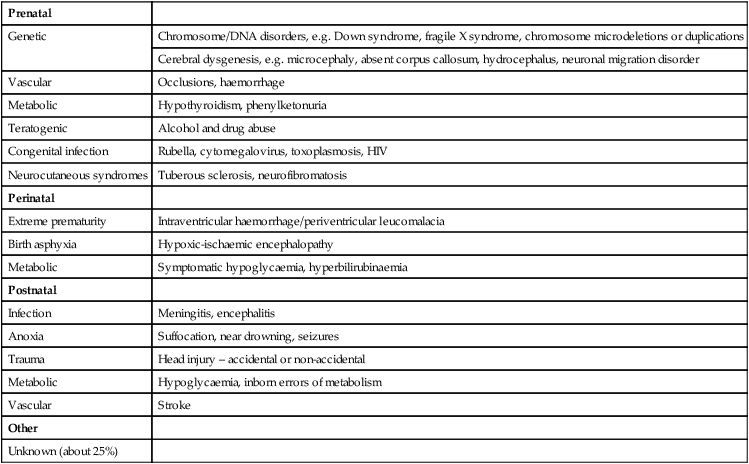
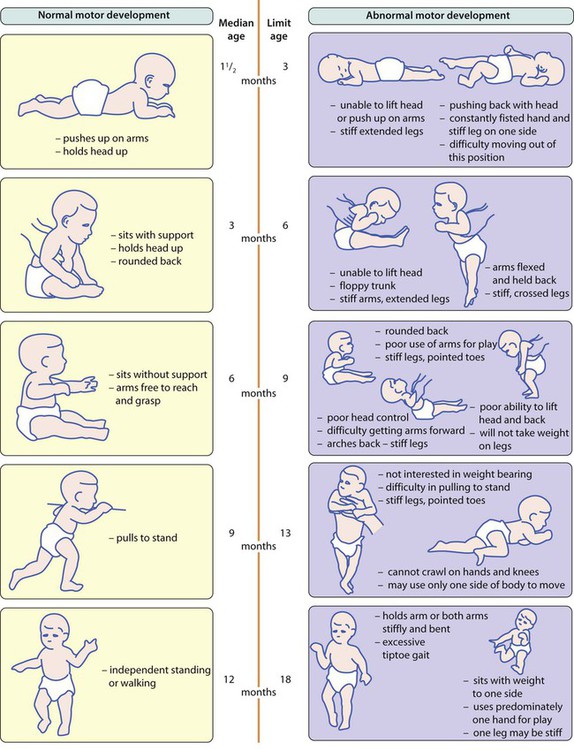
Any child whose development is delayed or disordered needs assessment to determine the cause and management. Neurodevelopmental problems present at all ages, with an increasing number now recognised antenatally (Table 4.1). Many are identified in the neonatal period because of abnormal neurology or dysmorphic features. During infancy and early childhood, problems often present at an age when a specific area of development is most rapid and prominent, i.e. motor problems during the first 18 months of age, speech and language problems between 18 months and 3 years and social and communication disorders between 2 and 4 years. Abnormal development may be caused not only by neurodevelopmental problems (Table 4.2) but also by ill health or if the child’s physical or psychological needs are not met. Table 4.1 Features that may suggest neurodevelopmental concerns by age Table 4.2 Conditions which cause abnormal development and learning difficulty The site and severity of brain damage influences the clinical outcome, i.e. whether specific or global developmental delay, learning and/or physical disability. When performing a clinical examination on a young child with a developmental problem: • Ask the parent what their child can and cannot do. Start at a level below what a child is likely to be able to do to retain confidence of the parent and child. • Observe the child from the first moment seen. • Make it fun. Your examination should be perceived as a game by the child, although they may not always follow your rules. • Toys to use are cubes, a ball, car, doll, pencil, paper, pegboard, miniature toys, picture book. Adapt their use to the child. • Formulate a developmental picture in terms of gross motor; vision and fine motor; hearing, speech and language; and social, emotional and behaviour. As you become more confident you will screen all these skills simultaneously. • At the end of developmental screening you should be able to describe what a child is able to do and what the child cannot do, if the abilities are within normal limits for age and, if not, which developmental fields are outside the normal range. • Clinical signs to look for that may aid diagnosis or guide investigation are: – patterns of growth: height, weight, head circumference with centile plotting – dysmorphic features: face, limbs, body proportions, cardiac, genitalia – skin: neurocutaneous stigmata, injuries, cleanliness – central nervous system examination: abnormal posture/symmetry, wasting, power and tone, deep tendon reflexes, clonus, plantar responses, sensory examination, cranial nerves – cardiovascular examination: abnormalities are associated with many dysmorphic syndromes – visual function and ocular abnormalities – hearing: by questioning parents about hearing and language development and checking if neonatal hearing screening was done – patterns of mobility, dexterity, hand dominance, communication and social skills, general behaviour Many examination findings can be predicted from observation of functional skills. The terminology can be confusing, but: • Delay – implies slow acquisition of all skills (global delay) or of one particular field or area of skill (specific delay), particularly in relation to developmental problems in the 0–5 years age group • Learning difficulty – used in relation to children of school age and may be cognitive, physical, both or relate to specific functional skills The following are agreed definitions: • Impairment – loss or abnormality of physiological function or anatomical structure • Disability – any restriction or lack of ability due to the impairment • Disadvantage – this results from the disability, and limits or prevents fulfilment of a normal role. It is situationally specific; a child with a learning disability may for example be a good skier or enjoy swimming. The pattern of abnormal development (global or specific) can be categorised as (Fig. 4.1): The severity can be categorised as: Other features of developmental delay are: • The gap between normal and abnormal development becomes greater with increasing age and therefore becomes more apparent over time (Fig. 4.2). • It may be the presentation of a wide variety of underlying conditions (Table 4.2). • The site and severity of brain damage influences the clinical outcome, i.e. whether there will be specific or global developmental delay, learning and/or physical disability. • It may be genetic, with important implications for the family. • There is a wide age band across which it can be normal to achieve a developmental skill. Limit ages denote beyond the normal range. The choice of investigations to identify the cause is influenced by the child’s age, the history and clinical findings (Table 4.3). In some children, no cause can be identified even after extensive investigation. Table 4.3 Investigations or assessment to consider for developmental delay Global developmental delay (also called early developmental impairment) implies delay in acquisition of all skill fields (gross motor, vision and fine motor, hearing and speech, and language and cognition, social/emotional and behaviour). It usually becomes apparent in the first 2 years of life. Global developmental delay is likely to be associated with cognitive difficulties, although these may only become apparent several years later. The presence of global developmental delay should always generate investigation into a possible cause such as those listed in Table 4.2. When children become older and the clinical picture is clearer, it is more appropriate to describe the individual difficulties such as learning disability, motor disorder and communication difficulty, rather than using the term global developmental delay. Causes of abnormal motor development include: • central motor deficit e.g. cerebral palsy • congenital myopathy/primary muscle disease • spinal cord lesions, e.g. spina bifida • global developmental delay, as in many syndromes or of unidentified cause. Late walking (>18 months old) may be caused by any of the above but also needs to be differentiated from children who display the normal locomotor variants of bottom-shuffling or commando crawling (see Ch. 3), where walking occurs later than with crawlers. • Abnormal limb and/or trunk posture and tone in infancy with delayed motor milestones (Fig. 4.3); may be accompanied by slowing of head growth • Feeding difficulties, with oromotor incoordination, slow feeding, gagging and vomiting • Abnormal gait once walking is achieved In CP, primitive reflexes, which facilitate the emergence of normal patterns of movement and which need to disappear for motor development to progress, may persist and become obligatory (see Ch. 3). The diagnosis is made by clinical examination, with particular attention to assessment of posture and the pattern of tone in the limbs and trunk, hand function and gait. There are three main clinical subtypes: spastic (90%), dyskinetic (6%) and ataxic (4%). A mixed pattern may occur. Functional ability is described using the Gross Motor Function Classification System (Table 4.4). Table 4.4 Gross Motor Function Classification System (GMFCS) See http://www.canchild.ca/en/measures/gmfcs.asp for further details (accessed January 2011).
Developmental problems and the child with special needs
Prenatal
Positive family history, e.g. affected siblings or family members; ethnicity, e.g. Tay–Sachs disease in Jewish parents
Antenatal screening tests, e.g. ultrasound including nuchal thickness and triple blood test for conditions such as Down syndrome, neural tube defects (spina bifida) and hydrocephalus. Amniocentesis for chromosomal disorders
Perinatal
Following birth asphyxia/neonatal encephalopathy
Preterm infants with intraventricular haemorrhage/periventricular leucomalacia, post-haemorrhagic hydrocephalus
Dysmorphic features
Abnormal neurological behaviour – tone, feeding, movement, seizures, visual inattention
Infancy
Global developmental delay
Delayed or asymmetric motor development
Vision or hearing concerns by parent or after screening
Neurocutaneous/dysmorphic features
Preschool
Speech and language delay
Abnormal gait, clumsy motor skills
Poor social communication skills
School age
Problems with balance and coordination
Learning difficulties
Attention control
Hyperactivity
Specific learning difficulties, e.g. dyslexia, dyspraxia
Social communication difficulties
Any age
Acquired brain injury, e.g. after meningitis, head injury
Loss of skills
Prenatal
Genetic
Chromosome/DNA disorders, e.g. Down syndrome, fragile X syndrome, chromosome microdeletions or duplications
Cerebral dysgenesis, e.g. microcephaly, absent corpus callosum, hydrocephalus, neuronal migration disorder
Vascular
Occlusions, haemorrhage
Metabolic
Hypothyroidism, phenylketonuria
Teratogenic
Alcohol and drug abuse
Congenital infection
Rubella, cytomegalovirus, toxoplasmosis, HIV
Neurocutaneous syndromes
Tuberous sclerosis, neurofibromatosis
Perinatal
Extreme prematurity
Intraventricular haemorrhage/periventricular leucomalacia
Birth asphyxia
Hypoxic-ischaemic encephalopathy
Metabolic
Symptomatic hypoglycaemia, hyperbilirubinaemia
Postnatal
Infection
Meningitis, encephalitis
Anoxia
Suffocation, near drowning, seizures
Trauma
Head injury – accidental or non-accidental
Metabolic
Hypoglycaemia, inborn errors of metabolism
Vascular
Stroke
Other
Unknown (about 25%)
Abnormal development – key concepts
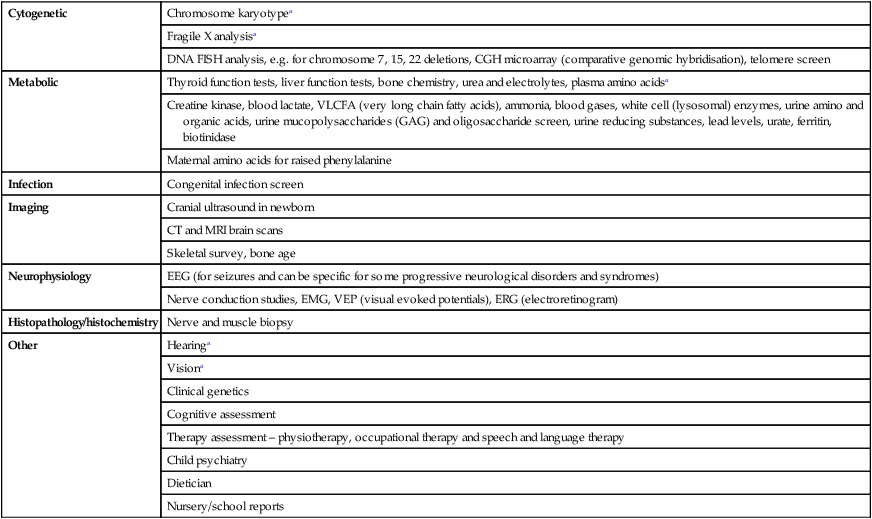
Cytogenetic
Chromosome karyotypea
Fragile X analysisa
DNA FISH analysis, e.g. for chromosome 7, 15, 22 deletions, CGH microarray (comparative genomic hybridisation), telomere screen
Metabolic
Thyroid function tests, liver function tests, bone chemistry, urea and electrolytes, plasma amino acidsa
Creatine kinase, blood lactate, VLCFA (very long chain fatty acids), ammonia, blood gases, white cell (lysosomal) enzymes, urine amino and organic acids, urine mucopolysaccharides (GAG) and oligosaccharide screen, urine reducing substances, lead levels, urate, ferritin, biotinidase
Maternal amino acids for raised phenylalanine
Infection
Congenital infection screen
Imaging
Cranial ultrasound in newborn
CT and MRI brain scans
Skeletal survey, bone age
Neurophysiology
EEG (for seizures and can be specific for some progressive neurological disorders and syndromes)
Nerve conduction studies, EMG, VEP (visual evoked potentials), ERG (electroretinogram)
Histopathology/histochemistry
Nerve and muscle biopsy
Other
Hearinga
Visiona
Clinical genetics
Cognitive assessment
Therapy assessment – physiotherapy, occupational therapy and speech and language therapy
Child psychiatry
Dietician
Nursery/school reports
Developmental delay
Abnormal motor development
Cerebral palsy (CP)
Clinical presentation
Level I
Walks without limitations
Level II
Walks with limitations
Level III
Walks using a handheld mobility device
Level IV
Self-mobility with limitations; may use powered mobility
Level V
Transported in a manual wheelchair
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Developmental problems and the child with special needs