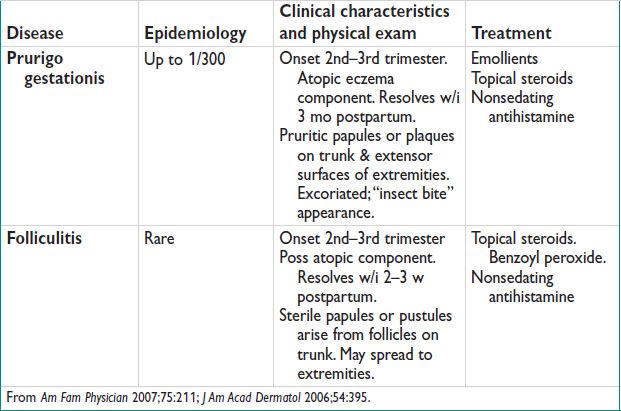
Lichen Sclerosus
Epidemiology
• Prevalence unk (often asymptomatic, underreported) (Obstet Gynecol Surv 2012;67:55)
• Bimodal distribution: Prepubertal & postmenopausal females, w/ a mean age btw the 5th & 6th decade (Obstet Gynecol 2008;111:1243)
• Risk of malig transformation to squamous cell carcinoma
Pathology
• Atrophic epidermis ± hyperkeratinization (typically due to persistent scratching), homogeneous collagen layer w/ underlying lymphocytic infiltrate, blunting of rete ridges
Etiology
• Autoimmune component & genetic predisposition suspected
• Hormonal influences (low estrogen) & local inflamm responses may also play a role
Clinical Characteristics
• Vulvar pruritis is most common symptom
May also present w/ vulvar irritation, pain, burning, dyspareunia
• Ddx: Psoriasis, lichen simplex chronicus, lichen planus, menopausal atrophy, candidiasis, autoimmune disorders such as vitiligo
Physical Exam (Obstet Gynecol Surv 2012;67:55)
• Exterior vulva thinned w/ a white plaque-like appearance, “cigarette paper”
• “Keyhole” distribution around vulva, introitus, & anus
• Excoriations & lichenification may be present due to persistent scratching
• Labia majora & minora may eventually lose distinction & fuse
• No vaginal involvement
Diagnostic Workup
• H&P exam
• Bx of affected area
• Rule out concurrent infxn
Treatment (Obstet Gynecol 2008;111:1243)
• Topical antihistamines for symptom relief
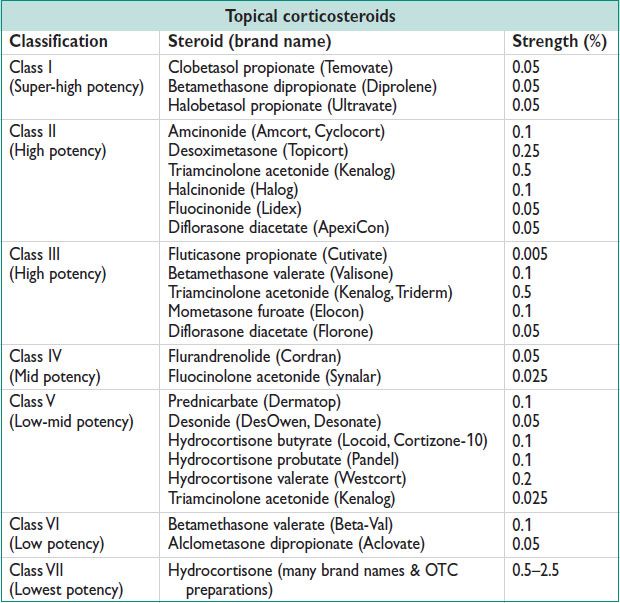
• High-dose topical steroids: Clobetasol 0.05% ointment nightly for 6–12 w, followed by maint 1–3×/w (1 of many rx regimens). See steroid chart, below.
• Topical retinoids for sev cases
• Topical tacrolimus, 0.1% ointment twice daily, or pimecrolimus 1% cream twice daily (do not use for extended periods)
• Triamcinolone injections: 2nd-line agents, indicated for persistent dz
• Pts should return in 3-mo intervals during initial rx stages, until stable
• Lifetime surveillance in 6–12-mo intervals recommended
LICHEN SIMPLEX CHRONICUS
Epidemiology (Dermatol Clin 2010;28:669)
• Common cause of vulvar pruritis: Prevalence is unk
• Personal &/or FHx of atopy is common
Pathophysiology
• Vulvar irritation (caused by heat, sweat, clothing, contact dermatitis, topical products, atopic conditions, infxn) → intense & persistent scratching → lichenification
Clinical Manifestations
• Pruritis
• Sleep disturbances, often due to pruritis & intense scratching
Physical Exam
• Erythematous thickened epidermis & scaly vulvar plaques
• Vulvar skin may be hyperpigmented or hypopigmented, & appear leathery
• Excoriations may be present
Diagnostic Workup/Studies
• Bx shows chronic inflamm changes, hyperkeratinization, acanthosis
Treatment (Obstet Gynecol 2005;105:1451)
• Vulvar hygiene, sitz baths
• Rx of underlying d/o (ie, infxn)
• Avoidance of scratching: Gloves at night, barrier creams, occlusive dressing, cold pack
• Topical steroids: Hydrocortisone 1% applied to affected area daily for mild dz. Betamethasone 0.05% or clobetasol 0.05% applied daily for mod–sev dz.
• Antihistamines: Diphenhydramine or hydroxyzine 25–100 mg po q4–6h prn
LICHEN PLANUS
Epidemiology
• Prevalence of ∼1% of women (Obstet Gynecol 2008;111:1243)
• Most common in the 5th–7th decade of life in females
Pathology
• Chronic inflamm changes, band-like dermal lymphocytic infiltrate, basal layer liquefactive necrosis, colloid bodies, acanthosis, hyperkeratinization
• Erosive lichen planus = most common form: Painful, desquamative, ulcerative lesions of vulva, vagina, & mucous membranes (including oral). Can form scar tissue, adhesions, or synechiae.
• Dev of squamous cell carcinoma is uncommon but poss
Etiology
• Presumed autoimmune process resulting in chronic inflammation
Clinical Manifestations (Am Fam Physician 2000;61:3319; Obstet Gynecol 2008;111:1243)
• “P’s”: Planar, Purple, Pruritic, Polygonal, Papules, & Plaques
• Pruritis is most common symptom
• May also present w/ vulvar or vaginal irritation, pain, burning, dyspareunia, discharge refrac to conventional rx
Physical Exam (Obstet Gynecol 2008;111:1243)
• Erythematous, shiny plaques of the vulva & occ the vagina
• May present w/ desquamation, ulcerations, & loss of architecture
• Wickham striae: White, lacy formation overlying papular lesions
• Bullae, ulceration, erosion in sev cases
• Oral & nongenital cutaneous lesions often coincide
Diagnostic Workup
• H&P exam
• Bx of affected area:
Immunofluorescence staining reveals basement membrane fibrinogen & IgM cytoids
Treatment (Obstet Gynecol Surv 2012;67:55)
• Symptom relief: Sitz baths, vulvar hygiene, barrier creams or petroleum jelly
• High-dose topical steroids: Clobetasol 0.05% cream applied nightly for 6–12 w, followed by maint 1–3×/w
• Topical tacrolimus, 0.1% ointment twice daily
• Triamcinolone injections
• Oral steroids for sev erosive dz: Prednisone 40 mg po daily × 1 w → taper
• Immune mediators (after failure of other methods): Methotrexate, azathioprine, cyclosporine, hydroxychloroquine
• Surgical procedures for adhesions or synechiae: Indicated when other treatments have failed
• Chronic condition, w/ relapsing-remitting course depending on resp to rx
• Routine yearly surveillance, as dev of squamous cell carcinoma is poss
SEBORRHEIC DERMATITIS
Epidemiology
• Overall prevalence unk
• Higher prevalence in immunocomp
• Most common in 3rd–4th decade of life
Etiology
• Lipophilic fungi of genus Malassezia implicated as potential pathogens
Grow in sebaceous glands
May be related to impaired immune resp
Clinical Characteristics and Physical Exam
• May present as asymptomatic plaques, as dandruff, or as pruritic, inflamed lesions where sebaceous glands are present
• Erythematous, yellow, oily scaly plaques in areas of sebaceous glands: Scalp, face, eyebrows, nasal folds, auricular surfaces, chest, back, body creases, vulva
Treatment (NEJM 2009;360:387)
• Antifungal meds: Ketoconazole 2% shampoo/foam/gel/cream BID for 4 w (evid is based on rx of scalp seborrheic dermatitis)
• Topical steroids to control itching, erythema: Hydrocortisone 1% daily or BID for 4 w, clobetasol 17-butyrate 0.05% cream daily or BID for 4 w, betamethasone dipropionate 0.05% lotion daily or BID for 4 w
• Calcineurin inhib: Pimecrolimus 1% cream BID for 4 w
• Recurrent dermatitis: Maint rx once or twice weekly
• Oral steroids or isotretinoin in sev cases; usually in the immunocomp or for refract dz
HIDRADENITIS SUPPURATIVA
Epidemiology (NEJM 2012;366:158)
• Prevalence 1–4%
• Most common in the 2nd–3rd decade of life
• 3 times more common in women
Etiology
• Often related to hormonal changes (hyperandrogenism), obesity, smoking, & meds
Pathophysiology
• Abn shedding of keratinocytes → terminal follicles in areas w/ apocrine glands become occluded & rupture → chronic inflammation, abscesses, sinus tract formation
Clinical Characteristics and Physical Exam (NEJM 2012;366:158)
• P/w erythematous, painful, nodular lesions, hyperhidrosis, odor
• Axilla & perineal regions most common, in addition to inguinal, perianal, & vulvar regions
• Less commonly p/w strictures, fistulae, lymphedema, osteomyelitis
• Nodular lesions form abscesses → resultant drainage causes sinus tracts & scarring
• Depression, decreased quality of life
• Hurley staging: Stage 1 – localized nodules or abscesses w/o scarring or tract formation, Stage 2 – recurrent nodules or abscesses w/ scarring or tract formation, Stage 3 – widespread nodules or abscesses w/ scarring & tracts
Treatment (Am Fam Physician 2005;72:1547)
• Initial treatments: Proper hygiene, use of neutral soaps, warm compresses, lightweight loose-fitting clothing, weight loss, smoking cessation
• Anti-inflamm meds
• Antiandrogen meds (spironolactone, drospirenone, finasteride)
• Topical Abx (tetracycline, clindamycin), oral Abx for more sev cases (clindamycin, rifampin)
• Retinoids (isotretinoin)
• Intralesional or oral steroids
• Immune mediators (infliximab, cyclosporine)
• Surgical treatments: Incision & drainage, wide local excision, laser excision, unroofing or debridement. Usually reserved for widespread & sev dz.
FOX-FORDYCE DISEASE
Epidemiology
• Infrequent; <1%
• Most common in 2nd–4th decade of life
• Predominance in females (female to male ratio 9:1)
Etiology
• Keratotic occlusion of apocrine glands → gland rupture & papular eruption → pruritis & chronic inflammation
• Apocrine gland involvement is necessary for dx
• Often related to humidity, obesity, hormones, stress
Clinical Characteristics
• May be asymptomatic, but most often p/w intense pruritis
• Affects the axilla, areolar, perineum, & pubic regions
• Multi small, darkened or flesh-colored papules
• May be a/w anhidrosis
• Acanthosis, or thickened skin, may be present
Treatment (J Pediatr Adolesc Gyn 2011;24:108)
• Combination OCP
• Topical steroids (0.05% desonide or 2.5% hydrocortisone once to twice daily)
• Topical or oral retinoids (0.025% tretinoin cream once daily)
• Topical or oral Abx
• Surgical excision of apocrine glands or liposuction curettage in sev cases
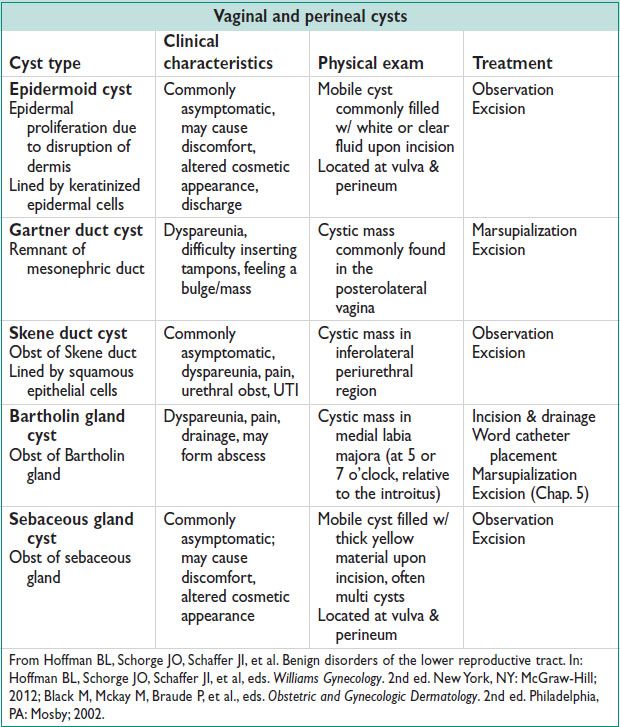
GYN-DERM CYSTS
COMMON DERMATOLOGIC MANIFESTATIONS OF SYSTEMIC DISEASE
Crohn’s Disease
• Approximately 30% of pts w/ Crohn’s dz have gyn-derm complications. See Ch. 15.
Findings: Vulvar edema, ulcerations, inflammation, granulomas, “knife cut” lesions or fissures. Inflammation, granulomas of the ovary & fallopian tube. Sinus tracts, enteric fistulae to the female reproductive tract.
Rx: Topical steroids, topical metronidazole, intralesion steroid injections, surgical correction of fistulae
Autoimmune Disorders (Obstet Gynecol 2008;111:1243)
• Thyroid dz, vitiligo, pernicious anemia, SLE, atopic dermatitis, & alopecia areata have been a/w lichen simplex chronicus, lichen sclerosus, & lichen planus
Behçet Disease
• Diagnostic criteria: Recurrent oral ulcers & 2 or more of the following: Recurrent genital ulceration, ocular lesions (uveitis), skin lesions, or positive pathergy testing
• Rule out infxn as source of ulceration, such as HSV, syphilis, HIV, chancroid
• Treatments: Topical or intralesional steroids; may require systemic rx
Stevens–Johnson Syndrome
• Systemic hypersensitivity rxn causing edema, sloughing, &/or necrosis of mucous membranes, including lower genital tract
• Usually caused by meds; can also be secondary to infxn
• Rx: D/c medication, supportive care, Abx, wound care; systemic steroids & IVIG may be helpful
Drug Reaction
• Small, hyperpigmented lesions, erythematous plaques or bullae
• Genital, oral, & facial lesions are most common
• Local rxn to systemic or local administration of some meds, most commonly: Tetracycline, phenolphthalein, sulfa medications, NSAIDs & ASA
• Resolves w/ discontinuation of the drug
Erythema Multiforme
• Small, cutaneous target-like lesions
• Bullae & erosions of the genital, oral, & ocular mucous membranes
• May be a/w infxn (HSV most common) or due to drug rxn
• Rule out infectious source (ie, HSV, syphilis, mycoplasma PNA)
• Rx: Withdrawal of causative agent, oral antihistamines, topical steroids, wound care, rx of infxn if present
< div class='tao-gold-member'>



