35 Dermatologic Conditions and Symptom Control
Skin disorders are often encountered in pediatric palliative care patients and can have both significant physical and emotional impact on a child’s well being. The skin is the largest organ in the body and accounts for 15% of a person’s body weight. Its major function is to provide protection from the external environment. This protection allows intimacy through the ability to touch and be touched. The skin is visible to the external world and its appearance can strongly affect a child’s self-image and a parent’s perception of the child. It is critical to identify dermatologic disorders and use an interdisciplinary team to take a whole-person approach to the treatment (Table 35-1).
TABLE 35-1 The Roles of Team Members in the Treatment of Wounds
| Disipline | Role |
|---|---|
| Child life specialist | |
| Spiritual counselor | |
| Nurse | Provide hand on medical care including dressing changes, medication administration, and repositioning |
| Certified nurses assistant | |
| Physician | |
| Psychiatrist | |
| Wound care specialist |
Psychosocial Impact of Dermatologic Conditions
In order to understand the psychosocial impact of skin disorders on pediatric palliative care patients, it is important to understand how skin disorders affect body image. Body image is a central part of self-concept and self-esteem, which is broadly defined as “the composite of thoughts, values, and feelings that one has for one’s physical and personal self at any given time.”1 Reactions to physical changes in the body often depend on whether the change involves an emotionally loaded body part or function or whether it results in a visible disfigurement. Physical appearance and attractiveness are major issues confronting adolescents, and their body image becomes a central aspect of their identity development.2 As a result of physical changes in appearance, others may stare or avoid looking at a child. Thereafter, the affected child may suffer emotionally and may withdraw socially. Although psychosocial research has been limited, studies have suggested that altered body image can interfere with daily functioning and has been associated with grief, anxiety, depression, social introversion, social avoidance behaviors, negative self-esteem, and avoidance of intimate relationships.3,4
A common diagnosis causing dermatologic symptoms in pediatric palliative care patients is cancer. The diagnosis of cancer is frequently associated with psychosocial and emotional issues. Studies indicate that children of all ages experience distress due to the effects of cancer treatment.5 A diagnosis of cancer often leads to multiple changes in physical appearance. These changes frequently include hair loss, presence of a central venous catheter, weight changes, and scars from surgery. The body-altering side effects of cancer have been reported by adolescents as the worst aspect of their disease.6 The adolescents’ sense of self-worth can be affected to such a degree that they withdraw socially from their friends and family. Physical changes due to cancer or its treatment can be devastating to a child’s self-image and can place the child at an increased risk for psychological and adjustment issues.7–9
Regardless of the underlying medical diagnosis, intact skin allows for intimacy and the ability to touch and be touched. Many teams that provide palliative care include massage or healing touch treatments to provide moments in which the child feels relaxed. Furthermore, touch is an important means for a child’s family to express their emotions and care. Any change in a child’s body image is likely to change closeness and intimacy through touch. Loss of intimacy may elicit psychological responses that become enduring and pathological, such as depressive symptoms and social anxiety. It should, however, be kept in mind that psychological responses subsequent to the development of dermatological conditions may not be simply the result of the skin condition, but be part of the child dealing with a life-threatening illness.10
Another important consideration is the psychological impact of pain that can be caused by the treatment of skin conditions. Painful treatments may include such things as changing wound dressings and physical therapy. The wound is a constant reminder that one’s body has been changed and nurses need to be attentive and sensitive to patient responses during wound care.11 Moreover, patients with wounds often report symptoms of depression and anxiety due to the pain.12 Another important factor to consider is that effects of dermatologic conditions such as pain, skin breakdown, and scarring may lead to limitation of motion and activity. These limitations may become a major cause of distress for the child.13 Young children particularly cope with distressing situations by engaging in play therapy. If the child’s play routine is limited due to a skin symptom, coping may be limited, too.
A skin disorder may also affect a child’s sense of self-competence as well as relationships with parents, siblings, or friends. Children and adolescents rely on different sources of social support. Children rely more on their parents and siblings, whereas adolescents obtain much of their support from peers. Peers are influential in the adolescents’ self-definition and self-evaluation. If adolescents become isolated from their peers, this may contribute to a sense of social deprivation and can put the adolescent at increased risk for depressive symptoms. Also, older adolescents facing changes in body image may be less likely to establish intimate relationships.14 If children or adolescents have less social contact, this may have significant implications on their ability to cope with the skin disease and their overall quality of life. It is important to facilitate and encourage connections between family members and peers. This can be done by open communication and by encouraging interactions with friends. These interactions may be face to face, through e-mails or social networking websites, or by phone calls between the child and his or her friends.
Adjustment to dermatologic symptoms is influenced by individual needs and coping behaviors, family support, palliative medicine treatment team, sex, age, and location of the injury.15 A powerful mediator of psychological problems is good communication among the care team, family, and child.16 Many of the problems experienced by the child require a combination of psychosocial and integrative medicine interventions. Possible psychological interventions are assisting the child to explore activities in which he or she is able to expose thoughts and feelings without feeling vulnerable. This includes validating their feelings, rationalizing, and developing a sense of acceptance. The treatment could be a combination of counseling and art therapy. Further, it may be helpful to allow the family to incorporate integrative modalities, such as guided imagery, healing touch, hypnosis, acupuncture, aromatherapy, or other mind-body skills. However, keep in mind that caring for children with skin conditions should not be separated from educating and helping families cope with the impact of the conditions.
Generalized Pruritus
Pruritus is an unpleasant cutaneous sensation that provokes the desire to scratch. It can be distressing and sometimes difficult to treat. It may lead to sleep disturbance, difficulty concentrating, anxiety, depression, and agitation. Left inadequately managed, it can have a significantly negative impact on a child’s quality of life.1
A recent position paper by the International Forum for the Study of Itch identifies six categories for the classification of pruritus based on its etiology: dermatologic disease, systemic disease, neurologic, psychiatric, and/or psychosomatic, mixed, and others.2 The causes of pruritus are numerous, and an extensive list is included in the paper published by the International Forum. Identifying the etiology of pruritus can be helpful when formulating a therapeutic approach. This chapter will address only the most common causes of pruritus in the palliative care setting.
Pathophysiology of pruritus
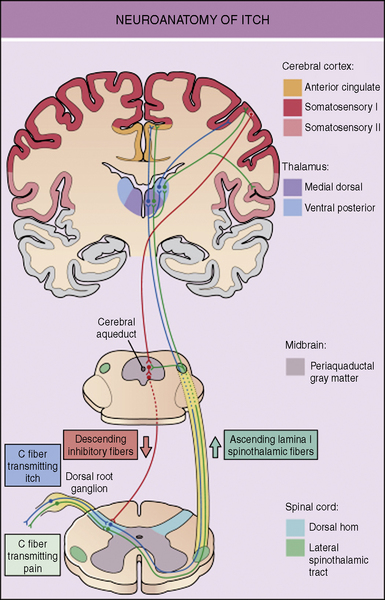
The neuronal pathways for the transmission of pruritus are thought to be closely related to, but distinct from, pain pathways. The skin is densely innervated by afferent C-fibers. These C-fibers transmit signals that lead to both the perception of pain and pruritus. About 80% of the C-fibers are activated by mechanical stimuli, being mechano-sensitive, while the remaining 20% are activated by chemical stimuli, including histamine, called mechano-insensitive. It is likely that some combinations of mechano-insensitive and mechano-sensitive C-fibers are responsible for the transmission of the itch signal to the dorsal root ganglia.3 Dorsal horn neurons then carry the itch signal up the spinal cord to the thalamus. Functional MRI imaging of the brain has shown activity in multiple areas of the brain, which encode sensory, emotional, attention-dependent, cognitive, and motivational aspects of itch.4 The perception of itch causes the response of scratching. Scratching creates a mild pain stimulus, which activates fast-conducting low-threshold nerve fibers that inhibit itch. It is believed that itch is under tonic inhibitory control of pain-related signals. It has also been demonstrated that μ-opioid receptor antagonists can have antipruritic effects but may intensify pain (Fig. 35-1).5–8
When pruritus is caused by dermatologic disease, peripheral C-fibers must be activated to transmit an itch signal. Histamine is the itch-stimulating substance, pruritogen, that is most typically targeted when treating itch, but there are other substances that stimulate itch including acetylcholine, bradykinin, endothelins, interleukins, leukotrienes, neurotrophins, prostaglandins, proteases, and kallikreins. These pruritogens can be released from various intracutaneous cell types. When these substances stimulate C-fibers, neuropeptides, such as substance P, are released. The neuropeptides then act on a variety of non-neuronal cell types, such as mast cells, which release further pruritogens thus creating a positive feedback loop and increases itch. Itch leads to scratching, which causes inflammation and the release of more pruritogens. Breaking this itch-scratch cycle can be particularly challenging. Recently investigators have identified ion channels, called transient receptor potential channels, that when stimulated, desensitize sensory afferents by depleting neuropeptides such as substance P. This interrupts the interplay between sensory neurons and mast cells and is a promising focus for the development of future therapies for pruritus.3 Capsaicin, which is being used in adults to treat pruritus, is an example of a medication that works through this mechanism.
The pathophysiology of pruritus caused by systemic disease is not fully understood, but it is often caused by increased levels of pruritogens, including endogenous and exogenous opioids. Itch of the neurological classification arises secondary to damage of nerves anywhere along the afferent pathway. Nerve damage can be seen in peripheral neuropathies, nerve compression or cerebral processes such as tumors, abscess, or thrombosis. Itch caused by psychiatric and/or psychosomatic disease can occur in disorders such as obsessive-compulsive disorder and parasitophobia. It is believed that both acute and chronic stress can trigger or enhance pruritus.9
Assessment
There are few assessment tools to evaluate the severity of pruritus in children. The tools that do exist are designed to be used in specific conditions, such as atopic dermatitis.10 In older children visual analog scales can be used to evaluate itch intensity. In the research setting a quantitative measure of pruritus can be obtained by a device that is able to measure the vibrations of the fingernails in the act of scratching.11
Management of Specific Conditions
It can be quite difficult to keep children from scratching areas that itch. Children often scratch irritated areas in their sleep or without thinking about it. It is crucial to keep a child’s fingernails cut short to prevent significant damage to the skin from scratching. Gloves or mittens can be place on children’s hands but they are often difficult to keep in place and can limit the child’s function. Case reports have suggested that hypnosis can be effective in reducing pruritus. This therapy may be a helpful adjuvant therapy for itch that is difficult to treat.12–14
Opioid-induced pruritus
Generalized pruritus that may localize to the face and trunk is a common complication of parenteral or neuraxial opioid administration. Pruritus can also be seen with the administration of oral opioids. It is difficult to estimate the incidence of opioids-induced pruritus in children for several reasons including limited data, variation between opioids and routes of administration, and lack of uniformity in methods of evaluation of pruritus. The incidence has been reported to be as high as 77% with parenteral administration of opioids in the postoperative setting.15 Among children with cancer-related pain, the incidence has been reported to be 28% with administration of oral or parenteral opioids.16 It is generally accepted that the incidence of pruritus is higher in neuroaxial administration of opioids than in parenteral administration. One 2006 study shows an incidence of 18% with parenteal opioids and 30% with epidural opioids.8
The mechanism of opioid-induced pruritus is not fully understood. It is known that orally and parenterally administered morphine can cause the release of histamine from mast cells, but fentanyl does not.17–19 Because both morphine and fentanyl are known to cause pruritus, this argues against histamine playing a significant role in opioid-induced pruritus. Furthermore, in studies done in primates, the administration of a histamine antagonist did not attenuate scratch induced by morphine.20 Any reported benefit of the use of H1-antihistamines in the treatment of opioid-induced pruritus is most likely related to the sedative properties of the medication. It is likely that opioid-induced pruritus is mediated centrally through μ-opioid receptors.20
In the initial management of pruritus caused by morphine, it may be helpful to change from morphine to an alternative opioid such as hydromorphone or fentanyl. If this is not effective, an opioid receptor antagonist can be administered in conjunction with the patient’s opioid. It is important, however, that the opioid antagonist be used in a low enough dose that it does not reverse the analgesia achieved by the opioid. Both naloxone and naltrexone have been studied. Naloxone can be administered at a starting dose of 0.25 mcg/kg/hr to 1 mcg/kg/hr. It is believed that doses of more than 2 mcg/kg/hr are likely to cause an unacceptable degree of reversal of the analgesic effect of the opioid. A pilot study done in children in sickle cell crisis found that patients tolerated co-administration of naloxone and morphine.5 A second study of 46 pediatric postoperative patients found that concomitant administration of low-dose naloxone and morphine PCA significantly reduced opioid-associated pruritus.15
Opioid agonist-antagonists, including nalbuphine and butorphanol, have also been studied as agents to reduce pruritus. Results of these studies have been mixed and studies are limited in the pediatric population. One study of 184 pediatric patients found that nalbuphine 50 mcg/kg IV given as a one-time dose was not effective in the treatment of postoperative opioid-induced pruritus.8 Nonetheless, additional studies are warranted. While these drugs have conceptual advantages over pure opioid antagonists in that they do not reverse the analgesic effect to the opioid, in combination with pure agonist opioids, they risk the precipitation of an opioid withdrawal syndrome and worsened pain. These medications act as antagonists at the μ-receptor and as agonists at the kappa-receptor. It appears that activation of kappa receptors attenuates morphine-induced itch without interfering with analgesia.21
Cancer-specific
The most effective treatment for cancer-related pruritus is anticancer therapy. In palliative care, however, many patients are responding poorly to or are no longer receiving disease- modifying therapies. In these patients, other approaches to the treatment of the pruritus must be identified. There is very limited data on the treatment of pruritus associated with cancer. In Hodgkin lymphoma there are case reports suggesting that the H2-receptor antagonist, cimetidine, is effective in treating pruritus.22 Corticosteroids typically given in conjunction with palliative chemotherapy can also relieve itch in late-stage Hodgkin lymphoma. Case series that have included pediatric patients suggested that pruritus caused by solid tumors may respond to the serotonin selective reuptake inhibitor paroxetine.23 While paroxetine’s antidepressant effects can take weeks to see, its antipruritic effects may be seen in as little as 24 hours after administration. In carcinoid tumors, blocking serotonin with a 5-HT3 receptor antagonist, such as odansetron, may be helpful.
Cholestastis
Cholestasis occurs in children of all ages, but it is particularly common in the neonatal period. The incidence of neonatal cholestasis is estimated to be approximately 1 in 2500 live births.24 The mechanism by which cholestasis causes pruritus is unclear, but elevated levels of circulating bile acids and endogenous opioids are both believed to play a role. It is also probable that the serotonin neurotransmitter system is involved. Recently the role that the serotonin neurotransmitter system plays in pruritus caused by cholestasis has been explored. There are studies in adults suggesting that the 5-HT3 receptor antagonist ondansetron, the selective serotonin reuptake inhibitors paroxetine and sertraline, and the noradrenalin and specific serotonin antagonist mirtazapine can be effective therapies.25–29 The pruritus of cholestasis is not thought to be mediated by histamine. Any relief that patients perceive with the administration of antihistamines is likely related to the sedating effects of the medication. It is of interest to note that if a patient progresses to liver failure, then pruritus often resolves.
First line therapy for pruritus caused by cholestasis is typically a medication directed at decreasing the level of circulating bile acids. Medications that can be used to achieve this result include nonabsorbable anion exchange resins such as cholestyramine, the hydrophilic bile acid ursodeoxycholic acid, and the hepatic enzyme inducers rifampin and phenobarbital.26,30–33 Nonabsorbable anion exchange resins are not effective in the case of complete biliary obstruction because the bile acids must reach the intestine for the medication to be effective. They are usually avoided in infants with portoenterostomy for biliary atresia because of concern about accumulation of the drug at the anastomosis causing obstruction.
If decreasing the level of circulating bile acids is ineffective or only partially effective, an opioid antagonist can be administered. The opioid antagonists naloxone, nalmefene, and naltrexone have all been shown to be helpful.34–37 Tolerance to these medications may develop over time, requiring dose escalation. Patients may experience symptoms of opioid withdrawal if they are treated with opioids; this can limit the medications’ usefulness.
Surgical interventions may also be helpful if medical management has not been successful and surgery makes sense within the goals of care. Procedures including partial external biliary diversion and terminal ileal exclusion have been shown to decrease pruritus in some children with intrahepatic cholestasis.38,39 In pruritus caused by extrahepatic disease, stenting the bile duct is often the best treatment for pruritus. In extreme cases of pruritus that is refractory to treatment and that is causing significant negative effects on a patient’s quality of life, liver transplant can be considered.
Uremia
Pruritus from uremia is seen in patients with chronic renal failure, but rarely in those with acute renal failure. The rate of pruritus is higher in patients receiving dialysis than in those not receiving dialysis. In adults, the presence of severe uremic pruritus is a predictive factor for death.40 The mechanism by which uremia causes pruritus is not fully understood, but as in other systemic illnesses it is likely caused by the accumulation of pruritrogens in the blood.
There is very little research that has been done in the pediatric population on pruritus secondary to uremia, so the treatment options are based on the adult literature. Initial management in patients on dialysis includes enhancing the dialysis regimen and correcting the patient’s calcium, phosphorus, and magnesium. Xerosis, which is very common in uremic patients, should be aggressively treated.41 If a patient is found to have hyperparathyroidism secondary to renal failure, pruritus can sometimes completely resolve after parathyroidectomy.42 Beyond these steps, UV-B therapy has been shown to be effective, but it has potential carcinogenic side effects.43 In recent studies, gabapentin has been shown to be a helpful treatment.44 Kappa-opioid receptor agonists have shown promise, but they have not been studied in children.45 As in pruritus caused by most other systemic diseases, the only role that antihistamines play in treatment are as sedatives.
Pruritus caused by renal failure can frequently be localized. This fact may allow for the use of topical agents. There has been recent interest in the use of capsaicin cream because it has been shown to deplete substance P from C-fibers when repeatedly applied.46 Its use may be limited in young children because it causes a burning sensation for the first few days it is applied. To make capsaicin more tolerable the skin can be anesthetized with a topical anesthetic, such as eutectic mixture of local anesthetics (EMLA), before the capsaicin is applied. Other topical agents, as well as systemic medications, are being studied for the treatment of pruritus caused by uremia, but the lack of clarity about the pathogenesis of the condition makes identifying new treatments difficult.
HIV/AIDS
Pruritus is very common in patients with HIV infection. It can be secondary to multiple etiologies, including infection, infestation, peripheral neuropathy, xerosis, a primary skin condition, systemic disease, drug reaction, or elevated levels of cytokines. A thorough evaluation for the most likely causes of the pruritus should be done and should direct treatment. Idiopathic HIV pruritus is uncommon and is diagnosed by the exclusion of other causes. Phototherapy can be an effective treatment, and one study in adults suggests that indomethacin may also be helpful47 (Table 35-2).
TABLE 35-2 Treatment of Pruritus by Cause
| Cause | Treatment |
|---|---|
| Xerosis | Oil-based emollients |
| Opioid induced | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|