4. Delivery Room Care*
Susan Niermeyer and Susan B. Clarke
The purpose of immediate delivery room care is to support the newborn’s respiratory and circulatory systems during the transition from fetal to neonatal life. Normal physiologic changes at birth include expansion of the lungs with air, initiation of gas exchange across the alveolar membrane, and closure of circulatory shunts that were necessary during intrauterine life. When delivery is complicated by perinatal conditions leading to asphyxia, the aim of resuscitation is to reverse hypoxia, hypercarbia, and acidosis. The survival and outcome of distressed newborns depend on timely and effective intervention in the first few minutes after birth.
Information in this chapter provides the reader with a clearer understanding of the physiologic events that take place in a distressed neonate and the current evidence and controversies behind the techniques used in delivery room resuscitation.
All resuscitation efforts begin with the basic techniques of thermal control, clearing of the airway, and stimulation of breathing. 2,38 Advanced resuscitation includes assessment of oxygenation, supplemental oxygen administration (if needed), bag-and-mask ventilation, endotracheal intubation, chest compressions, and use of medications and volume expansion. Delivery room emergencies may require the basic elements of resuscitation, as well as more advanced procedures that may be called for during stabilization in the delivery room and transitional nursery. Finally, the essential elements of successful resuscitation are care of the family, perinatal decision making, and teamwork among health care professionals.
PHYSIOLOGY
At birth, rapid physiologic transition from the intrauterine to extrauterine environment must be made. Effective, regular respirations should be initiated within 30 to 45 seconds of delivery. Environmental factors, such as a relatively cool ambient temperature and tactile stimulation, assist in initiating respiration. The changes in Pa o2 and Pa co2 resulting from clamping the umbilical cord affect chemoreceptors and aid in the reflexive initiation of respiration. The initial breath may generate from 20 to 70 cm H 2O of negative intrathoracic pressure to replace lung liquid with air inside the alveoli. 55 A rapid decrease in pulmonary vascular resistance and an increase in pulmonary blood flow occur after expansion of the lungs with air. This results in increased pulmonary perfusion and oxygenation. 54 Removal and absorption of fetal lung fluid is also necessary. Resorption of fetal lung liquid across the respiratory epithelium accelerates during labor, resulting in net clearance of liquid from the potential airspaces. 8 Colloid osmotic pressure and the relatively lower postnatal hydrostatic pressure of blood within the pulmonary circuit assist in absorbing alveolar fluid after delivery. During this process, fetal right-to-left shunts through the ductus arteriosus and foramen ovale gradually close (Figure 4-1; Table 4-1). 21
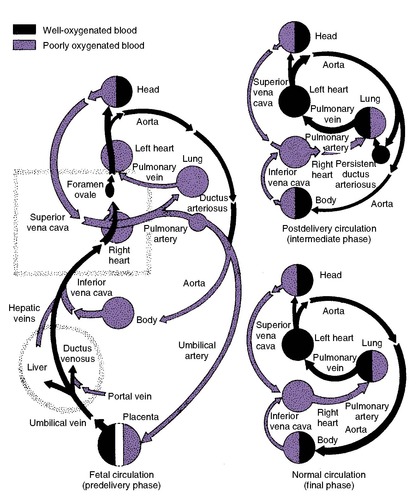 |
| FIGURE 4-1 (From Babson SG, Pernoll ML, Brenda GL: Diagnosis and management of the fetus and neonate at risk: a guide for team care, ed 4, St Louis, 1980, Mosby.) |
| Body Structure | Fetal Function | Extrauterine Function |
|---|---|---|
| Aorta | Carries oxygenated blood from left ventricle and deoxygenated blood from pulmonary arteries to fetal organs and placenta | Carries oxygenated blood from left ventricle into systemic circulation |
| Ductus venosus | Shunts most of the oxygenated blood from placenta to inferior vena cava | Disappears within 2 weeks after birth; becomes ligamentum venosum |
| Foramen ovale | Connects right and left atria; permits oxygenated blood from right atrium to bypass right ventricle and pulmonary circuit and go directly into left atrium | Functionally closes soon after birth; anatomically seals during childhood |
| Ductus arteriosus | Shunts blood from pulmonary artery directly into aorta | Functionally closes soon after birth; eventually becomes ligamentum arteriosum |
| Umbilical arteries and vein | Carry blood to and from placenta, the organ of respiration before birth | Clamped at birth, obliterating placental connections; become ligaments |
| Lungs | Distended with fluid; minimal pulmonary circulation; fetal respiratory movements | Expanded and aerated; pulmonary circulation allows CO 2 and O 2 exchange; organ of respiration |
ASPHYXIA AND APNEA
Asphyxia is defined as inadequate tissue perfusion that fails to meet the metabolic demands of the tissues for oxygen and waste removal. Asphyxia is characterized by progressive hypoxemia (↓ Po2), hypercarbia (↑ Pco2), and acidosis (↓ pH). 15 Hypoxic tissues convert from aerobic metabolism to anaerobic glycolysis, producing lactate and metabolic acidosis that is initially buffered by bicarbonate. 18 When the buffering capacity is exhausted, acidosis occurs. Acidosis and hypoxemia initially result in reflexive, compensatory cardiovascular changes. After early tachycardia, cardiac output decreases and generalized peripheral vasoconstriction occurs to maintain a blood pressure adequate for perfusion of vital organs. Prolonged asphyxia results in eventual bradycardia and hypotension as severe acidosis and cardiac failure occur.
Asphyxia may occur in utero or postnatally. In either circumstance, a well-defined series of respiratory events follow (Figure 4-2). 18 During primary apnea, respiratory movements cease after a brief period of rapid breathing. At the same time, heart rate falls and neuromuscular tone diminishes. Intrauterine asphyxia may result in the passage of meconium before birth. If the asphyxial insult continues, the heart rate falls further, blood pressure falls, hypotonia worsens, and a series of spontaneous deep gasps occur. Gasping continues but becomes weaker and more irregular and then finally ceases. After the last gasp, a period of secondary apnea begins. 18,38
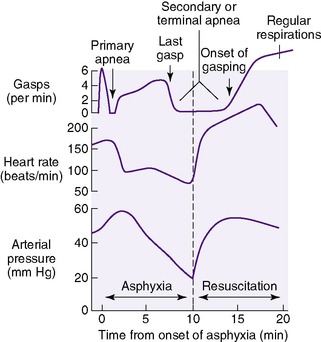 |
| FIGURE 4-2 (From Dawes GS: Foetal and neonatal physiology: a comparative study of the changes at birth, St Louis, 1968, Mosby.) |
Delivery may occur at any point during an asphyxial insult. If an infant is born during primary apnea, stimulation will usually induce respirations. If delivery occurs during secondary apnea, the infant will not respond to stimulation. Spontaneous respirations will not resume until resuscitation is initiated with assisted ventilation.1,18,38In the clinical setting, primary and secondary apnea are essentially indistinguishable from one another. The infant who is not breathing may have a heart rate below 100 beats/min and may be hypotonic. Thus any infant who is apneic at delivery must be assumed to be in secondary apnea, and resuscitation should begin immediately.
The longer the initiation of ventilation is delayed after an infant’s last gasp in secondary apnea, the longer the time necessary during resuscitation for return of the infant’s spontaneous respiration. For every 1-minute delay, the time to the first gasp increases by about 2 minutes and the time to the onset of spontaneous breathing is prolonged by more than 4 minutes.1 In the absence of effective resuscitation after delivery, apnea and decreased cardiac output result in progressive biochemical deterioration. 1,18
Severe fetal and neonatal asphyxia impair the physiologic transitions to extrauterine life. The normally high fetal pulmonary vascular resistance may not decrease in the presence of pulmonary hypoexpansion, persistent acidosis, and hypoxemia. Consequently, the pulmonary circuit continues to carry low volumes of blood. Oxygen transfer is impeded, perpetuating hypoxemia (Figure 4-3). 54 As part of persistent pulmonary hypertension of the newborn, normal closure of fetal shunts is delayed by high pulmonary vascular resistance and pulmonary hypoperfusion, hypoexpansion, and hypoxemia. This results in persistent right-to-left shunting through the ductus arteriosus and foramen ovale. Lung fluid clearance also may be delayed because of poor lung inflation or pulmonary hypoperfusion and hypoxemia. In addition, intraalveolar fluid may accumulate as a result of leakage from damaged pulmonary capillaries, resulting in pulmonary edema. With worsening hypoxemia and acidosis, myocardial function begins to fail, cardiac output falls, and perfusion decreases to vital body organs, including the brain, kidney, and intestine, setting the stage for postasphyxial injury of these organs. 15
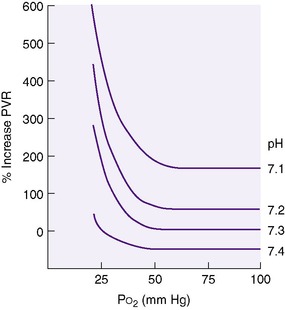 |
| FIGURE 4-3 (From Rudolph AM, Yuan S: Response of the pulmonary vasculature to hypoxia and H ion concentration changes, J Clin Invest 45:399, 1966.) |
RESUSCITATION OF THE NEWBORN
Preparation for Resuscitation
Immediate, effective resuscitation of the newborn infant can reduce or prevent morbidity and mortality. Much of neonatal resuscitation focuses on accurate assessment and initiation of ventilation. Application of basic procedures often is all that is necessary to successfully resuscitate a depressed infant. 49However, effective resuscitation requires anticipation, adequate preparation of equipment and personnel, and teamwork.6,50,74
Elements of the antepartum and intrapartum histories may identify the infant at risk for perinatal asphyxia (Box 4-1). However, any normal pregnancy may become high-risk at the onset of previously unexpected or undetected intrapartum complications, including maternal hemorrhage, cord prolapse, and meconium staining of the amniotic fluid. Although prevention, detection, and treatment of fetal asphyxia are the responsibilities of the obstetric team, therapeutic intervention should be coordinated between obstetric and neonatal services to ensure a timely delivery and effective, coordinated resuscitation.
BOX 4-1
Intrapartum Problems
• Fetal distress
• Persistent late decelerations
• Severe variable decelerations without baseline variability
• Bradycardia
• Meconium-stained amniotic fluid
• Cord prolapse
• Prolonged, unusual, or difficult labor
• Emergency operative or assisted delivery
• Breech presentation with vaginal delivery
• Narcotic administration to mother within 4 hours of delivery
Medical/Obstetric/Genetic Problems
• Diabetes mellitus
• Suspected or confirmed maternal infection
• Substance abuse
• Third trimester bleeding
• Pregnancy-induced hypertension
• Abnormal amniotic fluid volume
• Prolonged rupture of membranes
• Multiple gestation
• Low-birth-weight infant
• Prematurity
• Isoimmunization
• Fetal congenital anomalies
In the mid-1980s, the American Heart Association (AHA) and the American Academy of Pediatrics (AAP) addressed the need for a national training program for neonatal resuscitation in the United States by developing the Neonatal Resuscitation Program (NRP). The NRP provides the materials and training necessary for health care professionals to put into practice the scientific consensus established and updated periodically by the International Liaison Committee on Resuscitation (ILCOR). In 2000 and 2005, the guidelines were revised based on a rigorous process of evidence evaluation. 33,45 These changes have been incorporated into the fifth edition of the Textbook of Neonatal Resuscitation. 38 Evidence review is ongoing, and revised guidelines will be published in the Fall of 2010. The program’s widespread acceptance ensures consistent awareness of current scientific consensus, use of proper equipment, and preparation of personnel to work as a team using shared knowledge and performance skills.
The NRP recommends the following38
At every delivery, there should be at least one person whose only responsibility is the baby and who is capable of initiating resuscitation. Either that person or another who is immediately available should have the skills necessary to perform a complete resuscitation, including endotracheal intubation and administration of medications.
When a high-risk delivery is anticipated, two persons whose sole responsibility is resuscitation of the infant should be present and their roles designated in advance. Multiple births require a full team of personnel with complete equipment for each newborn.
The pediatric staff must be familiar with the prenatal and intrapartum history of the mother and fetus (see Box 4-1), because this information affects the initial level of resuscitation preparation.
Resuscitation equipment (Box 4-2) and drugs (Table 4-2) should always be readily available, functional, and assembled for immediate use in a designated location—ideally in a specific area of the delivery/birthing room. Consumable supplies and small equipment can be stored on specially constructed wall shelves or on a radiant warmer/intensive-care bed equipped with easily accessible storage (Figures 4-4 and 4-5).
BOX 4-2



 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Thermal Management
• Radiant warmer
• Warmed blankets or towels
• Infant stocking cap
• Food-grade plastic wrap or polyethylene bags
• Chemically activated warming pad
Airway
• Bulb syringe
• Mechanical suction
• Suction catheters—5-6, 8, 10, 14 Fr
• 8 Fr feeding tube and 20-mL syringe
• Meconium aspirator/suction device
• Shoulder roll
Breathing
• Bag-and-mask ventilation
• Oxygen source with flowmeter and tubing
• Neonatal resuscitation bag with 100% oxygen capability and manometer or pressure release valve and/or T-piece device
• Facemasks—newborn and premature sizes
• Oral airways—newborn and premature sizes
• Pulse oximeter
• Oxygen blender and compressed air source
• Intubation
• Laryngoscope with extra batteries
• Straight blades—No. 0 and No. 1 with extra bulbs
• Endotracheal tubes—2.5, 3.0, 3.5, 4.0 mm internal diameter
• Stylet
• Tape, skin preparation
• Scissors
• CO 2 detector
• Laryngeal mask airway
Circulation
• Stethoscope
• Wall clock or stopwatch
• Cord clamp
• Medications (see Table 4-2)
• Sterile gloves
• Alcohol sponges, povidone-iodine solution
• Umbilical vessel catheterization tray
• Umbilical catheters—3.5 and 5 Fr
• Three-way stopcocks
• Umbilical tape
• Suture material
• Intravenous catheters, tubing, fluid
• Needles—25, 23, 22, 20, 18 gauge
• Syringes—1, 3, 5, 10, 20, 50 mL
• Cardiorespiratory monitor
• Procedure light
| ETT, Endotracheal tube; IM, intramuscular; IV, intravenous. | |||||||
| Medication | Concentration to Administer | Dosage/Route | Total Dose/Infant | Rate/ Precautions | Indications for Use | ||
|---|---|---|---|---|---|---|---|
| WEIGHT (kg) | TOTAL mL | ||||||
| Epinephrine | 1:10,000 | 0.1-0.3 mL/kg IV (0.01-0.03 mg/kg) (preferred) | 1 | 0.1-0.3 | Give rapidly Use 2 different size syringes—one size for IV dosage and another size for ETT dosage | Heart rate <60 beats/min after 30 sec of adequate ventilation and chest compressions | |
| 2 | 0.2-0.6 | ||||||
| 3 | 0.3-0.9 | ||||||
| 4 | 0.4-1.2 | ||||||
| or | |||||||
| 0.3-1 mL/kg ET (0.03-0.1 mg/kg) | 1 | 0.3-1 | |||||
| 2 | 0.6-2 | ||||||
| 3 | 0.9-3 | ||||||
| 4 | 1.2-4 | ||||||
| WEIGHT (kg) | TOTAL mL | ||||||
| Volume expanders | Normal saline solution Lactated Ringer’s solution Whole blood | 10 mL/kg IV | 1 | 10 | Give over 5-10 min | Evidence of acute bleeding with signs of hypovolemia; poor response to resuscitation | |
| 2 | 20 | ||||||
| 3 | 30 | ||||||
| 4 | 40 | ||||||
| WEIGHT (kg) | TOTAL mg | TOTAL mL | |||||
| Naloxone hydrochloride | 1 mg/mL | 0.1 mL/kg (0.1 mg/kg) IV, IM | 1 | 0.1 | 0.1 | Severe respiratory depression and history of maternal narcotic administration within past 4 hr Give only after adequate ventilation and heart rate have been established | |
| 2 | 0.2 | 0.2 | |||||
| 3 | 0.3 | 0.3 | |||||
| 4 | 0.4 | 0.4 | |||||
Prepare for neonatal resuscitation by performing the following:
• Preheat the radiant warmer.
• Assemble consumable supplies: warm linens, bulb syringe, suction catheter, cord clamp, and appropriate personal protection.
• Check suction equipment for function, and set the vacuum regulator control not to exceed 100 mm Hg.
• Turn on the air/oxygen flow to the ventilation bag, and check all connections, flow-control valves, pressure-release valve, and manometer function to enable the ventilation bag to deliver up to 30 to 40 cm H 2O pressure. Ensure that an appropriate-size facemask is available.
• Check the laryngoscope for a bright light source and appropriate blades (size 0 for premature infants and size 1 for term infants); tighten the bulb.
• Check the availability of appropriate-size endotracheal tubes (2.5 to 4 mm internal diameter [ID]).
• Locate a stethoscope of appropriate size and confirm that it is functioning properly.
• Check the ancillary equipment (i.e., umbilical catheter supplies, intravenous [IV] solutions, unexpired resuscitation drugs).
• If the clinical situation warrants, draw up and label emergency medications for ready administration, using the estimated fetal weight, and obtain O-negative packed red blood cells for emergency transfusion.
The steps of neonatal resuscitation follow the standard ABCs of resuscitation:
A—Airway
B—Breathing
C—Circulation
With the ABCs as an overall framework for neonatal resuscitation, the components of the procedure can be examined sequentially:
A—Establish an airway
Position the infant
Clear secretions from the mouth, nose, and trachea (in some cases)
Perform endotracheal intubation, if necessary
B—Initiate breathing
Provide tactile stimulation
Provide free-flow oxygen, if indicated
Provide positive-pressure ventilation
C—Maintain circulation
Provide chest compressions
Administer epinephrine, volume expander
At each step of the resuscitation procedure, whether uncomplicated or extended, the cycle of evaluation/decision/action repeats. Evaluation includes simultaneous assessment of respirations, heart rate, and color (Figure 4-6).33 The importance of establishing an airway and initiating breathing cannot be overemphasized in neonatal resuscitation. Expansion of the lungs with air and adequate ventilation are the keys to successful resuscitation. Successful performance of these steps often obviates the need for further intervention, but inadequate lung expansion and ventilation cannot be overcome by performing chest compressions or administering medications.
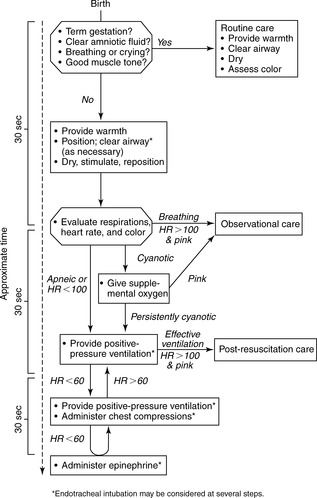 |
| FIGURE 4-6 (From Kattwinkel J, editor: Textbook of neonatal resuscitation, ed 5, Elk Grove Village, Ill, 2006, American Academy of Pediatrics and American Heart Association.) |
Apgar Score
The Apgar score provides a comprehensive, objective measure of the infant’s condition in the first minutes after birth (Figure 4-7). The Apgar score does not serve as an indicator of the need for resuscitation; rather, it quantifies an infant’s response to the extrauterine environment and resuscitative measures. In term and preterm infants, the Apgar score remains a valuable predictor of infants who will need ongoing support in the immediate perinatal period and those who are at higher mortality risk in the neonatal period. 17
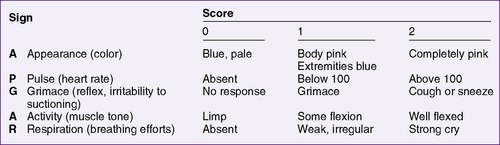 |
| FIGURE 4-7 (From Butterfield J, Covey M: Practical epigram of the Apgar score, JAMA 181:353, 1962.) |
Although perinatal asphyxia may be associated with low Apgar scores, it is possible for an infant to have a low Apgar score without having asphyxia. 35 For example, an infant born to a mother who received general anesthesia may be flaccid and have depressed reflexes and poor respiratory efforts. Such infants usually respond rapidly to bag-and-mask ventilation, and no further intervention is necessary. However, an infant may have an equally low Apgar score as a result of intrauterine asphyxia and may require prolonged resuscitative efforts. An infant with a mid-range Apgar score between 6 and 7 may be using homeostatic mechanisms to maintain an adequate central blood pressure and cardiac output. Apgar scores should be assigned at 1 and 5 minutes, and every 5 minutes thereafter until the score is 7 or greater. A complete description of the timing and nature of resuscitative steps is vital to interpreting a low Apgar score. 3
Although the Apgar score is not used to guide resuscitation, the experienced clinician performs a rapid visual assessment of an infant at the moment of birth. This rapid assessment incorporates two elements from the Apgar score, as well as two key questions that influence the overall conduct of the resuscitation.
Rapid Assessment After Birth
In the first few seconds after birth, a rapid visual assessment of the baby should be performed to answer the following questions, 33which can be summarized by the acronym TART:
• Is the baby term?
• Is the amniotic fluid clear?
• Is the baby breathing or crying? ( respiratory effort)
• Is there good muscle tone?
If the answer to all of these questions is “yes,” the baby can remain with the mother to receive routine care as described in the Routine Care and Initial Steps of Resuscitation section that follows.
If the answer to any of the questions is “no,” the infant should be evaluated under a radiant heat source during the initial steps of resuscitation. If meconium is present, the vigor of the infant may alter the initial steps.
If meconium is present, evaluate the vigor of the infant:
• Does the baby have strong respiratory efforts?
• Is there good muscle tone?
• Is the heart rate greater than 100 beats/min?
If the answer to all of the questions is “yes,” the airway may be cleared as described in the Position and Clear the Airway section. If the answer to any of the questions is “no,” the infant requires endotracheal intubation for suctioning.38,74 In this circumstance, return to the initial steps of resuscitation and complete them after intubation for suctioning of meconium.
Routine Care and Initial Steps of Resuscitation
The care of every infant at birth includes (1) warmth, (2) clearing the airway (positioning and suctioning as necessary), and (3) support of breathing with drying and tactile stimulation.
Whether part of routine care or during the initial steps of resuscitation, many of the actions can be performed simultaneously, especially if more than one person is caring for the infant.
PROVIDE WARMTH
• Dry the infant, and place him or her directly on the mother’s chest; cover both with warm linen (routine care).
or
• Place the infant under a radiant heat source, drying him or her thoroughly and removing the wet linen.
or
POSITION AND CLEAR THE AIRWAY (AS NECESSARY)
• Ensure that the infant’s neck is slightly extended when positioning him or her on the mother’s chest; wipe secretions from the mouth and nose, or suction with a bulb syringe as necessary (routine care).
or
• Position the infant supine and flat with the neck slightly extended. A rolled blanket or towel may be used under the shoulders.
• Turn the head (or the head and body) to the side to allow secretions to pool in the cheek, and then remove with a bulb syringe or suction catheter. Suction the mouth and then the nose to clear the airway. The mouth is suctioned first to clear the largest volume of secretions; when the nasopharynx is suctioned, a reflex cough, sneeze, or cry often results. Deep pharyngeal suction in an infant not requiring positive-pressure ventilation or intubation should not be performed during the first few minutes after birth to avoid vagal stimulation, resultant bradycardia, and delay in rise in Pa o2. 13,22
or
• If meconium is present, evaluate the vigor of the infant before drying (as described earlier) to decide if endotracheal intubation is needed. 74
STIMULATE AND REPOSITION
• Provide tactile stimulation by briefly rubbing the back or gently slapping or flicking the feet.
• Continue gentle rubbing of trunk, extremities, or head to support early respiratory efforts in the newborn.
• Keep the head and neck in a slightly extended position to maintain an open airway.
Evaluate the Infant
Evaluation of the infant is a continuous, ongoing process. Subsequent action is guided by evaluation during each step of resuscitation and decisions about whether the response is adequate.
EVALUATE RESPIRATIONS
• Rate and depth of respirations (chest wall movement, air exchange) must be adequate; apnea and gasping respirations both require positive-pressure ventilation.
EVALUATE HEART RATE
• The heart rate should be greater than 100 beats/min. Feel the base of the umbilical cord or listen over the left side of the chest with a stethoscope to count the heart rate. Count the heart rate in 6 seconds and multiply by 10 for the beats per minute. Indicate each beat (for other team members) by tapping the forefinger on the bed or tapping the thumb and index finger together.
EVALUATE COLOR
• Give free-flow oxygen if the infant is breathing but remains centrally cyanotic. Peripheral cyanosis (acrocyanosis) is not an indication for supplemental oxygen. The goal of oxygen administration should be normoxia, not hyperoxia. 66
Positive-Pressure Ventilation
Indications for positive-pressure ventilation in the newborn infant include the following:
• Apnea or gasping respirations despite a brief period of tactile stimulation
• A heart rate less than 100 beats/min
• Central cyanosis despite free-flow oxygen
Prolonged tactile stimulation or administration of supplemental oxygen to a baby who is not breathing effectively or who has a heart rate less than 100 beats/min only delays appropriate treatment. If supplemental oxygen is unavailable, positive-pressure ventilation should be initiated with room air. 45When supplemental oxygen is available, it should be administered with the goal of achieving normoxia and avoiding hyperoxia. Ongoing research in animals and humans has demonstrated that room air is equivalent to 100% oxygen for positive-pressure ventilation in many newly born infants. The exclusive use of 100% oxygen for postnatal resuscitation, as previously recommended, can result in hyperoxia and predisposition to changes induced by generation of oxygen free radicals.64,65 The concentration and duration of supplemental oxygen administration should be individualized to patient needs. Pulse oximetry, initiated as soon as feasible, can help guide oxygen administration.19,63Ideally, it should be possible to administer oxygen in concentrations from 21% to 100% in the delivery setting. This has special importance for preterm infants who are more vulnerable to oxygen injury yet may need concentrations greater than 21%.59,70
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree