41 Cystic Fibrosis
reaching upward toward the sky
With permission from “The Breathing Room: The Art of Living with Cystic Fibrosis” at www.thebreathingroom.org
Cystic fibrosis (CF) is a well-known disease to most pediatricians and pediatric palliative care clinicians. Given the degree of familiarity about the disease for the readers of this volume, this chapter intertwines two goals: to provide an updated view of CF in the early twenty-first century and to propose an ideal and somewhat novel model for integrating the pediatric palliative care team into the care of patients and families affected by CF. While the population of adults with CF will soon be larger than that of children,1 this chapter does not include a comprehensive discussion of the palliative care of adults with CF because most are cared for in adult CF centers with different challenges and resources.
As described further in this chapter, the typical patterns of care for patients with CF have historically presented predictable barriers to the successful integration of palliative care. Understanding of the natural history, the changing epidemiology and cultural understanding, and the perceived and actual physical and psychosocial burden of the disease will help palliative care providers better understand how to integrate their clinical expertise and psychosocial support of the patient and family into the established and successful CF model of clinical care. Further, this can be done without disrupting the typically well-established relationships between patients and their families with the CF care team. While the proposed value added model described later and outlined in Table 41-1, may not seem distinctive to many palliative care providers,2 it will be seen as a novel approach by most CF care teams.
TABLE 41-1 Help From Palliative Care Teams
| How can the pediatric palliative care team help the CF team care for children, adolescents and families with CF throughout the lifespan? |
|---|
| Before the diagnosis is made |
| Help the CF care team design and implement a supportive and compassionate approach to those who have a positive newborn screen for CF, realizing that a positive screen can be a distressing experience even if the infant is not diagnosed with the disease. |
| At the time of diagnosis |
|---|
| Help the CF team care develop strategies to mitigate the impact of parental grief following the disclosure of a life-threatening diagnosis in an infant, especially if the infant is apparently healthy. |
| During routine care |
|---|
| Help the CF care team anticipate and prepare for emotional reactions to the first hospitalization, which can trigger parental anxiety about disease progression and mortality. |
| Help the CF care team become comfortable with discussions of mortality throughout the patient’s life, so that the team is prepared for inevitable questions and discussion with patients and families. |
| As the disease progresses |
|---|
| Help the CF care team gain expertise in the assessment and treatment of symptoms throughout the lifespan, including expertise in pain management and assessment of non-pulmonary, non-GI symptoms, such as fatigue or anxiety. |
| Help the CF care team plan a comprehensive roadmap for the decisions, which will be faced by patients, parents, and clinicians in the now rarer instance of a childhood or adolescent death, including anticipatory guidance about the use of aggressive technologies. |
| Offer the CF care team assistance with planning and carrying out the process of transplant decision making. (See Table 41-3.) |
| Offer expertise and experience with managing symptoms and end of life care in different settings, such as at home or through pediatric hospice services, if available. |
| After the death of the child or adolescent |
|---|
| Offer comprehensive bereavement services for the family, siblings, and medical providers. |
An Overview
Cystic fibrosis is a life-threatening genetic disease with an incidence of 1 in 3200 live births in the United States. An estimated 30,000 people are now living with CF in North America.3 CF is a multisystem disease resulting from mutations in the cystic fibrosis transmembrane regulator (CFTR) gene, causing abnormal chloride ion transport across epithelial cells lining the airways, pancreatic ducts, gastrointestinal tract, and reproductive organs. This abnormal transport leads to dehydrated and viscous secretions. Clinical manifestations of this defect include recurrent respiratory infections, nutritional deficiencies related to malabsorption from pancreatic exocrine insufficiency, intestinal obstruction, hepatobiliary disease, diabetes, and male azospermia.4 The natural history of CF is a progressive decline in lung function caused by recurrent infection, inflammation, and bronchial obstruction leading to bronchiectasis and subsequent ongoing inflammation, infection, and airway damage. Chronic inflammation and infection of the airways accounts for most of the morbidity in CF, and the vast majority of patients with CF eventually die from respiratory failure.5
Survival in CF has increased dramatically over time due to advancements in medical care. Additionally, lung transplantation for advanced CF lung disease is an option that may extend life or improve quality of life for select patients. The population of patients with CF is shifting: In 2007, 45% of patients with CF in the United States were adults, and the median predicted survival for patients with CF reached 37.1 years.1 Despite advancements in care and longer survival, patients with CF and their families endure the challenges associated with a chronic disease, including the burden of numerous therapies and disease exacerbations, the knowledge of a limited lifespan, the responsibility of complex decision making regarding lung transplant and other intensive treatments, and the stigma and reproductive choices associated with a genetic disease.
The Current Approach
From the time of diagnosis, daily therapies are prescribed for maintenance of respiratory health and nutritional status, and emphasis is placed on psychosocial implications of chronic disease. To facilitate management of this complex disease, an interdisciplinary approach to care is believed to be essential. In addition to receiving standard medical care from a primary care provider, many patients attend quarterly or more frequent clinic visits and receive hospital care at specialty CF care centers. CF care teams are composed of multiple providers, including physicians, nurses, social workers, dietitians, physical therapists, and respiratory therapists (Table 41-2).
TABLE 41-2 Structure of Outpatient CF Care
| Provider | Frequency of visits | Role in CF care |
|---|---|---|
| Primary care physician | Variable | |
| CF physician | At least quarterly | |
| Nurse | At least quarterly | |
| Dietitian | At least annually | |
| Social worker | At least annually | Address psychosocial issues, including coping with chronic disease, family structure, educational issues, financial and insurance concerns |
| Physical therapist | At least annually | |
| Respiratory therapist | At least quarterly | |
| Other consultants* | Variable | Provide services according to discipline and patient need |
* Other specialty areas may include allergy/immunology, anesthesiology, cardiology, endocrinology, gastroenterology, genetics, genetic counseling, infectious disease, neonatology, obstetrics/gynecology, otolaryngology, psychiatry, psychology, pulmonology, radiology, surgery, and urology.
Adapted from Orenstein DM, Rosenstein BJ, Stern RC. Cystic Fibrosis Medical Care. Lippincott Williams & Williams, Philadelphia, 2000.
For patients with CF, basic respiratory care involves a combination of airway clearance techniques to enhance removal of mucus from the lower airways, aerosolized therapies to facilitate mucus clearance by altering its viscosity, various antimicrobial and anti-inflammatory medications, and exercise.3 Many of these therapies are time-consuming and may prove challenging to maintain. A survey of adults with CF revealed that they spend an average of nearly 2 hours per day on respiratory therapies.6 Children with CF require close supervision from caregivers, and even older patients often need assistance from caregivers to carry out respiratory therapies and other treatments.7 With progressive disease, oxygen may be used with exertion, during sleep, and ultimately constantly.8 Non-invasive positive pressure ventilation may be recommended for patients with hypercarbia and respiratory insufficiency, and has gained favor over time as a bridging therapy for patients awaiting lung transplantation.9
Respiratory exacerbations of CF manifest in many ways, with symptoms including increased cough and sputum production, dyspnea, fatigue, fever, chest pain, hemoptysis, sleep disturbance, and weight loss. Concomitant changes in physiologic measures, including chest exam, oxygen saturation, spirometry measures, and weight, may occur. Treatment of respiratory exacerbations involves additional therapies and hospitalization for severe exacerbations for many patients. Intravenous antibiotics are commonly used, often in combination given the challenges of combating virulent and often drug-resistant CF pathogens such as Pseudomonas aeruginosa, oxacillin-resistant Staphylococcus aureus, and Burkholderia cepacia, and therapeutic drug monitoring and surveillance for associated toxicities is necessary. Intensification of aerosolized therapies and airway clearance techniques during exacerbations is also common practice.5 Complications of progressive CF lung disease, including pneumothorax, hemoptysis, hypercapnia, pulmonary hypertension, and respiratory failure, prompt more extensive evaluation and treatment, sometimes in the intensive care unit.10
Patients with pancreatic insufficiency must take pancreatic enzyme supplements with food to enhance digestion and reduce the likelihood of intestinal obstruction, as well as taking fat soluble vitamin supplements to prevent vitamin deficiencies. Anti-reflux medications and laxatives are also commonly prescribed. Because of the established correlation between nutritional status and lung function, great emphasis is placed on appropriate growth for children and weight maintenance in adults.11 For many patients who struggle to gain weight, nutritional supplements, appetite stimulants, and enteral feedings may become mainstays of therapy. Additionally, approximately one-fifth of adults develop CF-related diabetes, and most of these patients ultimately require frequent glucose monitoring and treatment with insulin injections.9
cleanse me of this putridity within.
As my body soaks in that which
is meant to remove the foul poison,
the pills, the needles, the aerosols pulls me
down like an anchor in a deep sea,
it controls who I am, my time, my life.
I should be floating in a bubble bath
of elegance, luxury, perfection.
Instead, there are no bubbles, they all burst.
It’s just me and this bath of disease.
With permission from “The Breathing Room: The Art of Living with Cystic Fibrosis” at www.thebreathingroom.org
Understanding the Goals of Care for the CF Team
When the CFTR gene was initially described in 1989, many believed a cure for the disease was imminent.12 This hope led to great optimism regarding the approach to care for children with CF. Now, 20 years later, no cure is on the horizon.13 Widespread and consistent application of chronic treatments by patients and their families has led to increasing life expectancy, and even in the face of the discouraging results of research into a cure from gene transfer, most patients, families, and clinicians maintain an attitude of vigorous optimism toward the disease. CF clinicians generally adopt an enthusiastic approach, becoming cheerleaders for their patients, emphasizing the optimistic increases in life expectancy and vigorously encouraging their patients to keep up hope for improved survival and quality of life. This attitude is in part a response to the outdated image of CF among the general public as a killer of children, in part a strategy to encourage adherence to the increasingly time-consuming daily CF regimen, and in part an antidote to the unpredictable, waxing and waning course of the illness. CF care teams maintain a position of enthusiastic optimism in coaching patients and their families to continue the work associated with a life with CF.
Although there is much to be optimistic about with regard to CF, in some circumstances this optimism may inhibit frank discussion of the reality of life with CF. Despite the ever-expanding life expectancy, people with CF still experience significant suffering.14–24 The disease burden and physical and psychosocial distress can be seen:
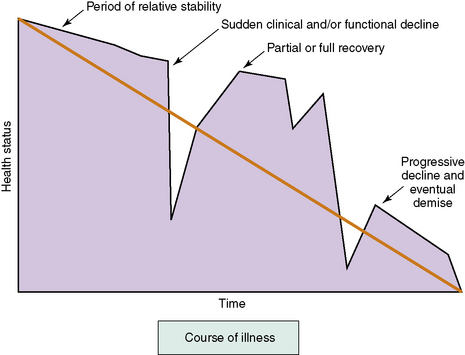
Unfortunately, even the most experienced CF medical provider is unable to predict when these episodes of acute illness and loss may occur,25 and the disease carries a large degree of uncertainty.26 Many patients with CF experience acute de-compensations, recoveries, and periods of relative stability, usually superimposed upon a gradual downward trajectory in lung function (Fig. 41-1). The functional ability of patients over time often mirrors this course. Most patients will have periodic setbacks, and while some of these setbacks will include a complete recovery, others may result in a decline in functional ability. The palliative care provider should recognize how this uncertainty and progressive loss of function will affect children and adults with CF, their families, and their medical providers.
Integrating the Palliative Care Team into CF Care
Given this mixed picture of CF, discussing palliative care has been a challenge. In the view of many CF care teams, palliative care is associated only with the medical interventions aimed at providing comfort at the end of life. As a result, specific palliative care interventions, including therapies directed at managing symptoms present in those with mild to moderate disease, are often not introduced until the patient is clearly at the end of life—often too late for the patient and family to derive the benefit of the palliative care team’s expertise. Palliative care, clearly differentiated from end of life care and integrated with curative and restorative measures, offers the best chance at limiting the burden of disease, maximizing quality of life at all stages of illness, and providing effective support to children and adults with CF and their families.27 A value added model, when provided as consulting expertise in a programmatic approach, may succeed in these situations when a more conventional approach has failed and help limit the reluctance of the CF team to involve palliative services.
The model is based on using the expertise of the palliative care team to help the CF team address the grief that often accompanies the diagnosis of a chronic life-threatening illness. It continues by emphasizing the expertise of the palliative care team in assessing and managing symptoms and assessing the burdens of treatment relative to the benefit. As symptoms progress in CF, the palliative care team assists the CF team in responding to the inevitable questions about mortality both from parents and children. The palliative team uses its expertise in discussing these matters to help the CF team be more comfortable with these issues in the context of the generally successful CF routine care. As the disease progresses, the palliative care team should further support the family in the decision making process about lung transplantation, including discussions of mortality and the benefits and burdens of an intensive treatment in pursuing the goals of care, because the current model of care leaves little time for discussion of the use of intensive measures and the goals of care.28 The palliative care team will then act in a traditional way—it is only during this phase of care that many CF teams traditionally contact the pediatric palliative care team—to assist the CF team in managing end-stage symptoms and providing high quality care at the end of life. Finally, the palliative care team will help in the bereavement process, not only for the family, but also for the long-serving and dedicated members of the CF care team (see Table 41-1).
Before the diagnosis is made
CF is a well-characterized genetic disorder with an autosomal recessive pattern of inheritance. Although most living patients were diagnosed following the appearance of symptoms or due to the diagnosis of a sibling, most new diagnoses will now be made through newborn screening programs, which have spread rapidly across the United States in the past few years.29 The advent of newborn screening using immunoreactive typsinogen and/or DNA analysis has resulted in a population of asymptomatic patients diagnosed in the first month of life. Earlier diagnosis has led to some improved clinical outcomes,30,31 but does carry some associated risks for families, including psychological impact of false negative and false positive results and implications of diagnosis of a genetic disease.2,32,33 Because of their experience with breaking bad news and with helping families manage the grief that may accompany the news, palliative care teams are in a good position to help CF care teams design a compassionate program for revealing the diagnosis to those parents of newborns who have a positive screen and then a confirmatory genetic analysis or sweat test.34
At the time of diagnosis
As the diagnosis is given, families must process not only the shock of the diagnosis but also the beginning of a complex new care regimen, which must be followed every day if the benefit of newborn screening is to be realized.35,36 The obvious parallel for the palliative care team is a new and unexpected diagnosis of cancer in a child, with the rapid institution of a complex and toxic therapy. While the side effects of therapy are less in the newly diagnosed child with CF, the shock and grief may be similar. CF care teams are accomplished at helping families with this news, but the advent of newborn screening brings a new group to light in the CF clinic: the largely asymptomatic child with a genetic diagnosis. The change in the experience of the diagnosis may offer an opportunity for the palliative care team to approach the CF care team with an offer to help it do the best possible job in supporting this new type of patient. While we do not recommend the palliative care team have direct contact with the family at the time of diagnosis, the interdisciplinary expertise of the palliative care team may prove to be useful to the CF care team during this time.
During routine care
Two events in particular may provide room for the palliative care team to assist the CF care team. The first is preparing it to respond to the patient and family when they bring up the limited life expectancy of someone diagnosed with CF. Many CF clinicians prefer never to talk about this issue, or to brush it aside with discussion of the progress in CF. However, it is clear that patients, especially by adolescence, recognize this issue and may very well want to talk about it.37,38 In the popular culture, CF is viewed as a progressive killer of children: movies, books, and novels about CF are inevitably tragic and highly melodramatic.39–43 Popular narratives about CF may be years out of date,44 and it is a trope that anyone portrayed on television with CF will die before the show ends. Patients and families swim in this cultural sea, and so are exposed to this inaccurate but tight link of CF with childhood death. This may cause them to be reluctant to disclose their disease to others, even friends, and so may cut them off from sources of social support that could have a positive effect of quality of life.45 Palliative care teams, as outsiders to the CF community, may be able to help the CF care team counter these popular images of CF and replace them with a more accurate portrayal of patients with CF as deeply courageous and dedicated in the face of a difficult but potentially life-affirming situation. CF medical providers do not want to be surprised when an adolescent asks about mortality, and the palliative care team may be able to develop an educational approach that explores the range of developmentally appropriate responses to a patient’s questions.
The palliative care team may also have a window of opportunity to assist the CF care team at the time of the first hospitalization for a pulmonary exacerbation. Even when most children were symptomatic at the time of diagnosis, the first pulmonary exacerbation was a time of substantial stress, during which the reality of disease progression had to be faced.46,47 Now, in the era of the asymptomatic diagnosis via newborn screening, the first exacerbation can stir up considerable anxiety for parents, and they may interpret it as a sign of more rapid decline of the child. Of course, it is the intensive and preventive approach to CF that is the cause of both the treatment for pulmonary exacerbation and the increase in life expectancy, and habituating the family to the routine of careful surveillance and vigorous treatment of any fall from the pulmonary baseline is an important goal. CF teams may not recognize the increased symbolic meaning of this first exacerbation in the era of newborn screening, as pulmonary exacerbations and their treatment are routine for the teams.
As the disease progresses
Assessment and Management of CF-Related Symptoms
Distressing symptoms are common in patients with CF14,16,19,23,24,48 and are known to increase as lung disease progresses,17,49,50 but little research defines the impact of symptoms on quality of life or on the end of life experience of these patients. General principles of symptom assessment and management can be applied to the CF population, and the interdisciplinary nature of CF care should allow for regular attention to symptoms with both physiologic and non-organic origins. Attention must be paid to the psychological impact of symptoms, particularly respiratory symptoms, as their increasing frequency and intensity typically denotes disease progression.
Respiratory Symptoms
Respiratory symptoms, such as cough and dyspnea, may be minimal or only intermittent during infancy and early childhood but in most patients progress steadily, with periods of increased cough and dyspnea occurring during respiratory exacerbations. Cough is necessary for clearance of respiratory secretions, and is encouraged in this setting, but excessive cough may be distressing and disruptive. Aerosolized therapies and airway clearance techniques facilitate cough, and are routinely recommended for maintenance of health and are intensified during respiratory exacerbations. While these treatments are intended to reduce chronic respiratory symptoms, they are thought to be burdensome by many patients.6 This perception is due in part to the extensive amount of time required to complete such treatments, but clinical experience suggests that they may also cause distressing symptoms such as pain, dyspnea, sleep disturbance, and urinary incontinence. Treatment of increased cough includes use of aerosols and airway clearance therapies, antibiotics for infection, and specific treatments for other common causes of cough, including gastroesophageal reflux disease, sinus disease, asthma, and allergies. While most pulmonologists who treat patients with CF discourage the use of antitussives because of their negative impact on airway clearance, these agents may be helpful in managing distressing cough under certain circumstances.
Hemoptysis may occur in association with cough, particularly with lower respiratory infections. Small-volume hemoptysis is generally managed with antibiotics, correction of bleeding disorders, and cautious use of or temporary suspension of aerosols and airway clearance therapies. Massive hemoptysis, which is more than 240 mL in 24 hours or recurrent bleeding of more than 100 mL per day, occurs in approximately 1% of children with CF and is unrelated to severity of lung disease. It is also associated with other respiratory complications and has a high likelihood of recurrence.51,52 Bronchial artery embolization is used for acute treatment, but recurrent and unremitting end-stage hemoptysis may require sedation and the use of dark towels and linens to minimize the sight of blood, which may help lessen the anxiety of patients, caregivers, and medical providers.
Dyspnea is commonly reported as CF lung disease progresses50 and is likely to be the most distressing symptom near the end of life. This complex symptom is related to: increased ventilatory demand due to increased dead space in abnormal CF lungs, increased respiratory effort to move air through dilated and obstructed airways, and increased muscle force required for maintenance of normal ventilation because of abnormal airway resistance and flattening of the diaphragm by hyperinflated lungs.53 In addition, the interplay between dyspnea and anxiety can be complicated.54,55 There are many approaches to the treatment of dyspnea. Enhancing airway clearance and treating infection and inflammation with standard CF therapies is a standard strategy, which may reduce acute or subacute dyspnea, ideally returning the patient back to their baseline respiratory status. With disease progression, dyspnea may become less responsive to such treatments.
For those with chronic dyspnea and more advanced lung disease, physical therapy to improve conditioning may be helpful. Respiratory support, including the use of oxygen to support gas exchange, may reduce the sensation of dyspnea. Oxygen may be used with exertion, during sleep, and on a continual basis later in the course of disease. The route of administration is typically nasal cannula, although some patients prefer to use face masks during periods of acute illness. The use of positive airway pressure for management of dyspnea, hypoxemia, and hypercapnia was typically avoided in the past because of poor outcomes of patients receiving these treatments.56–58 Applying positive pressure to airways that are abnormally dilated and impacted with thick mucus makes airway clearance, which is critical to management of respiratory infection, more difficult. In addition, ventilator modes and settings that combat hypercapnia due to respiratory failure in advanced CF lung disease are uncomfortable and typically necessitate sedative medications that interfere with the patient’s ability to communicate. However, the use of non-invasive positive pressure ventilation, typically bi-level positive airway pressure (BiPAP), has gained favor for patients with sleep disturbance and daytime fatigue and as a bridging therapy for patients with respiratory insufficiency awaiting lung transplantation.59,60 Full respiratory support with intubation and mechanical ventilation may also be considered for some patients with reversible causes of respiratory failure and for transplant candidates.61,62 The decision to use these treatments must be made with the knowledge that, while they may provide relief of severe dyspnea and may prolong life for those whose goal is to receive a lung transplant, their use has many associated risks that must be understood by patients and caregivers.
Decreasing the sensation of dyspnea using oral and intravenous opioids and benzodiazepines may be considered for patients with advanced lung disease. Opioids decrease respiratory drive and may act locally in the lungs to relieve dyspnea.63 However, despite evidence that these medications can be used safely in patients with respiratory diseases,54 concerns about respiratory depression in patients with advanced CF lung disease have been described and may act as barriers to effective palliation of dyspnea.10,49,53,64 Aerosolized opioids are sometimes offered, but small studies of their use to treat dyspnea do not suggest universal efficacy.63,65,66 Given the demonstrated efficacy of opioids in relieving dyspnea, concerns about their use may be alleviated by starting with very low oral or intravenous doses and titrating to effect, monitoring closely for undesirable secondary effects. This strategy also allows the patient, caregivers, and medical providers time to become more comfortable with the use of opioids to treat dyspnea. Other supportive and adjunctive therapies, including lowering ambient temperature or blowing cool air with fans, maintaining cooler ambient temperatures, positioning, relaxation techniques, and psychotherapy, may be beneficial for some patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree