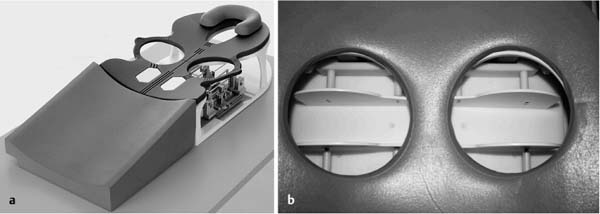
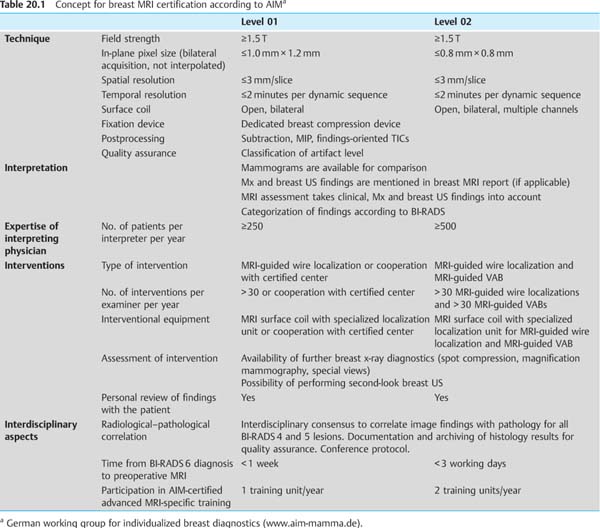
20 Current Standing, Problems, and Perspectives of Breast MRI It is indisputable that due to the development of open surface coils with multiple channel systems and integrated compression devices, as well as the improvement of especially the spatial resolution in all three planes, HR breast MRI has become the most reliable imaging modality in breast diagnostics (Fig. 20.1). A technically and methodologically flawless breast MRI allows not only the detection of invasive breast carcinomas from a diameter of 3–4 mm (sensitivity 94%–98%) but also the detection of intraductal carcinomas with the highest accuracy (sensitivity 85%–90%). The technique thus demonstrates itself to be significantly superior to x-ray mammography and breast ultrasonography, especially in the early detection of breast cancer (pTis, pT1a, pT1b). The specificity of breast MRI, which has occasionally been criticized as being too low, is good when the examination is performed with appropriate quality and evaluated with high expertise. At 70%–80% it lies in the same range as that of other breast imaging techniques. Breast MRI examination is therefore generally to be recommended in those cases in which other breast imaging techniques (x-ray mammography, breast ultrasonography) have significant limitations. This is especially true for x-ray mammography when parenchymal density is high (ACR density III and IV) and the sensitivity is therefore reduced to as little as less than 50%. This limitation does not apply to breast MRI because the mammographic density of parenchyma does not correlate with parenchymal enhancement on MRI. Currently acknowledged indications for the performance of breast MRI particularly take into account women who have an increased risk of having or developing breast cancer. As a result, the following indications for the performance of breast MRI are generally accepted standards of good practice: Apart from the indications listed above, breast MRI is often implemented as an efficacious “problem solver” when there are ambiguous findings in x-ray mammography and/or breast ultrasound. In such a situation, breast MRI often provides a definitive directive for or against performing a percutaneous biopsy. Breast MRI is the method of choice for the evaluation of prosthesis complications. The use of special sequence protocols that allow selective imaging of the various prosthesis components, and the capability for slice imaging in multiple planes, make breast MRI superior to other imaging modalities for this indication (see chapter 14). The combination of bilateral digital x-ray mammography in the MLO projection with HR breast MRI (known as the Göttingen Optipack) is presently the examination protocol with the most reliable detection of breast carcinomas and the least possible parenchymal radiation dose. This combination allows the detection of both invasive and intraductal carcinomas with very high sensitivity. Fig. 20.1a, b Open surface coil. Indispensable for high-quality breast MRI. a Open surface coil. b Breast compression device. Motion artifacts used to be a major limiting factor in the diagnostic value of breast MRI examinations. This methodological problem has been almost completely eliminated by the construction of open surface coils combined with a breast compression device. A diagnostic limitation that remains is the occasional disturbing early enhancement of parenchyma due to hormonal stimulation, which can sometimes mask small tumor lesions. This “physiological problem” decreases breast MRI transparency and diagnostic reliability similarly to the way high parenchymal density does for mammography. Fortunately, in the relevant age group this phenomenon (early physiological enhancement) is only seen in fewer than 5% of all examined women. For comparison, mammographically dense breast tissue (ACR type III and IV) is found in at least 50% of these same women. Potential solutions to alleviate this problem in breast MRI are the generation of earliest subtraction slice images, and the discontinuation of stimulating hormone therapies, or even temporary antiestrogen therapy before performing the examination. A further, solvable problem is the variable image quality seen area-wide. The main cause of suboptimal image quality is the use of substandard MRI equipment and methods. The excellent results for detection of DCIS in breast MRI, for example, can only be achieved when the examination is performed with a high matrix (512 × 512) and without motion artifacts. The application of an adequate certification process which records and tests quality-relevant criteria for MRI equipment and examiner expertise can improve the current standards. Accordingly, the German working group for individualized breast diagnostics (AIM, a registered association) has prepared a conceptual plan for accreditation of physicians providing breast MRI examinations. This certification program provides for two expertise levels and is expressly individual-orientated and intended only for medical specialists (Table 20.1).
Current Standing
Value of Breast MRI
Indications for Breast MRI
 Differentiation between a postoperative scar and breast cancer recurrence after breast-conserving surgery (BCS)
Differentiation between a postoperative scar and breast cancer recurrence after breast-conserving surgery (BCS)
 Search for the primary tumor in the presence of a CUP syndrome
Search for the primary tumor in the presence of a CUP syndrome
 Early breast cancer diagnostics in women with a high-risk profile
Early breast cancer diagnostics in women with a high-risk profile
 Preoperative local staging in women with histologically verified breast cancer
Preoperative local staging in women with histologically verified breast cancer
 Response monitoring in women undergoing neoadjuvant chemotherapy
Response monitoring in women undergoing neoadjuvant chemotherapy
Göttingen Optipack
Problems and Solutions
Limitations of Breast MRI
Certification
< div class='tao-gold-member'>
Current Standing, Problems, and Perspectives of Breast MRI
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree