3 | Criteria and Rules |
Methods of Locating Points
Each acupuncture point has a specific method by which it is located. It is possible to find points using various methods, but precise localization is imperative for therapeutic success. Anatomical landmarks, such as for example bone processi and bone fossae, skin folds, hairlines, nipples, the navel, etc., offer great points of reference. The relation to such a structure allows the practitioner to identify a point if it is located in its vicinity. Palpation of the presumed location of an acupuncture point is important, because sensitivity to touch is considerably higher at the point location than it is at its surroundings.
Areas that are painful to touch correspond to classical acupuncture points particularly in the case of painful disorders of the musculoskeletal system, neurological disorders, and disorders of internal organs.
A-shi points (see p. 34) are especially painful to touch but do not correspond to classical acupuncture points. They are applied as local points in addition to specific distant points.
On the following pages, various methods of locating points will be explained in detail.
Locating Points Based on Anatomical Landmarks
Acupuncture points are located through their relation to prominent anatomical landmarks such as spinous processes, pubic crest, muscle insertions and muscle bellies, palpable tendons, but also eyebrows, hair lines, joint folds, mammillae, and the navel. For example, CV-12 is located exactly in between the inferior end of the sternum (xiphoid process) and the navel.
Proportional Measurement Using Cun
Proportional measuring of point locations using cun is helpful with points that are located far from anatomical landmarks. These points can be found through their proportional distance (cun) to a point of reference. Cun are the relative measurements of the patient (Fig. 30).
The therapist may use his/her own cun measurement if it matches the cun of the patient. An obvious deviation will cause difficulties for the assessment. In this case, the cun measuring unit only offers a rough orientation. In daily practice, the cun measurement is never used by itself. If a point is located with the use of cun it has to be confirmed through palpation.
The Proportional Body Cun
The size of body parts is of fixed proportion, which can be described in cun. Traditional Chinese Medicine (TCM) lists exact cun proportions for the distance between body parts and areas:
— Navel—xiphoid process | 8 cun |
— Navel—pubic crest | 5 cun |
— Elbow—wrist fold | 12 cun |
— Greater trochanter—center of the patella | 19 cun |
— Center of the patella—lateral malleolus | 16 cun |
— Both nipples | 8 cun |
— Nipple—midline (ren mai) | 4 cun |
— Distance between ribs | 1 cun |
— Frontal—dorsal hairline along the midline (ren mai) | 12 cun |
Locating Points by Taking a Particular Position
The patient takes a particular position or positions body parts in a way that favors the location of points. For example, LI-11 can be found at the lateral end of the elbow fold when flexing the arm 90°.
Locating Points by Measuring Skin Resistance
At many acupuncture points the skin resistance is low compared to its surroundings. The use of commercial point-locating equipment (resistance meter) is based on this fact. This equipment records the change in skin resistance acoustically or through a light-emitting diode. However, it is not possible to exactly locate all points using lowered skin resistance. Also, skin resistance changes due to various factors such as perspiration, changes in body temperature, and changes in skin moisture. Thus, this method is at times not specific enough. The method might be recommended for less experienced therapists, but, ultimately, the development of adequate palpating skills is preferred.
Measuring skin resistance is useful in ear acupuncture because the skin resistance of the auricle changes particularly in those areas that are associated with diseased organs. This assists in making the correct diagnosis. In addition, locating points with point-locating equipment is helpful in this area due to the density of points.
Using Other Acupuncture Points as Reference Points
Frequently, points are found via other points that are easily located. After locating these reference points, cun are used to find the actual points. For example, LI-10 is usually located via LI-11 (see above).
Palpation
Usually various methods of locating points are combined in daily practice, such as referring to anatomical landmarks and the subsequent confirmation through palpation. In regard to palpation, the following has to be taken into consideration:
— Adequate pressure is required (stroking is not palpating);
— The area used for palpation cannot be too large (tip of index finger instead of thumb);
— Patient response during palpation needs to be considered (further inquiry: “Where do you feel the greatest [pressure] change?”).
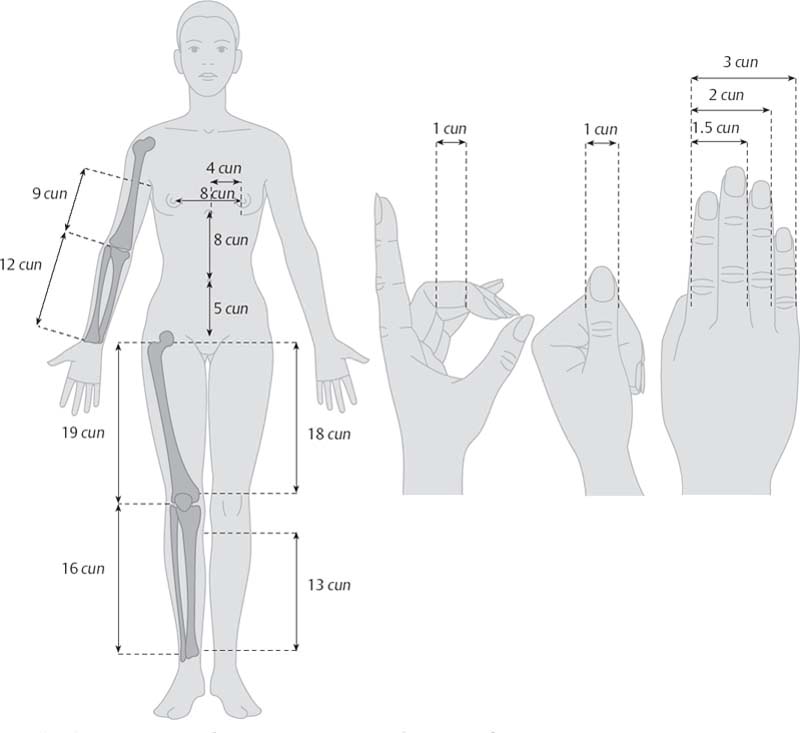
Fig. 30 The Chinese propotional measurement cun (according to Kampik)
Prerequisites For Acupuncture Therapy
Although the TCM and Western medical views may be opposing, the successful application of acupuncture treatment in the West requires:
• Thorough diagnosis by means of Western medicine
• Detailed analysis of symptoms based on TCM concepts by following the system of traditional diagnosis criteria, and the categorization of symptoms by channels and organs leading to a TCM pattern diagnosis
• Creating a treatment plan based on valid therapy principles of acupuncture while considering the totality of the disorder
• Knowledge of the 12 regular channels and their pathways, of the two extraordinary channels ren mai and du mai, their relation to each other, and of the location pattern of the most important, specific points
• Precise location of the correct points, exact needle technique and insertion depth, and the adequate form of point stimulation (tonifying, sedating).
Effects and Reactions
 Scientific Background
Scientific Background
The effects of acupuncture are always the result of various components. When working with acupuncture therapy, placebo effects and suggestion have to be taken into consideration. The allegation made by conventional medicine that the effects of acupuncture are exclusively based on these influences cannot be upheld today. Scientific research has shown the effects of acupuncture therapy in the following areas:
• Peripheral and central nervous system (CNS) Analgesic effects of acupuncture; three levels of effectiveness:
1. Level of the spinal cord: Segmental inhibition of pain stimuli through nonpainful stimuli from neuromuscular spindles (by the neurotransmitters enkephalin and dynorphin).
2. Level of the midbrain (raphe nuclei): Descending inhibition of the posterior horn neurons through the monoamines serotonin and norepinephrine.
3. Level of the hypothalamus and pituitary gland: Stimulating the secretion of beta-endorphins into blood and CSF.
• Humoral/endocrine effect.
Not only does acupuncture affect the secretion of endorphins and serotonin, it also affects the body’s cortisol production (Sheng et al. 1980, Stux and Pomeranz 1988) and blood circulation (e. g., by activating the vasoactive intestinal polypeptide [VIP]). It affects muscles through musculoactive substances and by influencing kinetic chains. Changes in the immune response include the increase of lymphocytes and a decrease in IgE.
The Effects of Acupuncture on Pain
The Canadian neurophysiologist B. Pomeranz (University of Toronto) explains the analgesic effects of acupuncture as a process that takes place on three levels: The pain stimulus is sent from its origin, for example the uterus (labor pain), through nerve fibers to the posterior horn of the spinal cord. Here the pain stimulus is transferred to a neuron, which sends it on to the thalamus and ultimately to the cerebral cortex, where pain is perceived. The neurotransmitters at the synapses of the posterior horns are enkephalin and dynorphin. In the midbrain, hypothalamus, or thalamus, other endorphins (beta-endorphin, dynorphin) transmit the stimulus. It is in these synapses that the pain can be modulated.
The insertion and manipulation of the acupuncture needle stimulates the pressure receptors and mechanoreceptors which are located in the muscles.
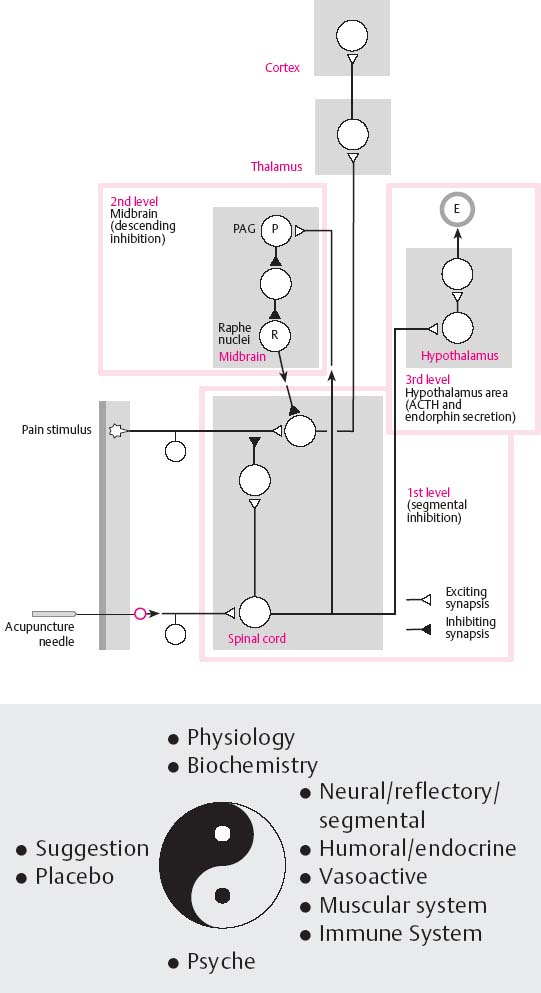
Fig. 31 Acupuncture analgesia—effects and effect model (according to Pomeranz)
The general effects on the organism following needle insertion can be divided into local, segmental, and central effects.
• Local reactions
The needle causes a microinjury. In contrast to a hollow needle (injection cannula), the tissue is merely pushed apart and tissue damage is minimal. Nociceptors are usually not directly affected. Tissue hormones (mediators) are released which immediately repair the injury and initiate a fast biochemical chain reaction. Mediators of this chain reaction are histamine, serotonin, kinin, lymphokines, leukotrienes, and prostaglandins. Their effects are locally limited and include dilation of capillary loops, increase of capillary permeability, changes in the interstitial environment, and, thus, stimulation of the nociceptors, activation of nonspecific immune response, and attraction of leukocytes and Langerhans cells. In many patients, this local reaction can be recognized as redness in the area of needle insertion.
Mediators rarely cause more far-reaching reactions, such as orthostatic dysregulation brought on by histamine (can lead to cardiogenic shock), stimulation of intestinal peristalsis caused by serotonin, intensification of insulin effects that will lead to lower blood sugar levels caused by kinin, inhibition of gastric juice secretion caused by prostaglandin A, dilation of bronchial muscles caused by prostaglandin E, constriction of bronchial muscles caused by prostaglandin F, and increased chance of uterine contractions caused by prostaglandins E and F.
• Regional (segmental) reactions
The afferent nerve fibers of the stimulated pain receptors induce a regional reaction. Pain receptors, mechanoreceptors, and pressure receptors transmit the information via the dorsal root of the spinal nerves to the corresponding spinal cord segment. After a relay in the gray matter of the posterior horns, synapses pass on information to other nerve cells. This transfer influences regions of the adjacent segments of the spinal cord. An additional information impulse travels to the brain where the central reaction occurs. Regional reaction is primarily prompted on the level of the spinal cord segment and its adjacent segments. It is an independent information exchange that is merely modified by the central reaction. Primary sites of exchange are interneurons that relate information within one segment and respond back to the point of insertion via efferent neurons and neurons of the autonomic nervous system. Simultaneously, Head zones involve the related internal organs. Neurons can intensify or change impulses (e. g., stimulating impulses can be changed to inhibiting impulses). Some impulses are blocked while others are intensified and directly transmitted (gate control theory by Melzack and Wall).
Vascular dilatation is a regional effect of acupuncture. This leads to improved blood supply to the area, which is usually perceived as a sensation of warmth. Muscle relaxation (perceived as general relaxation) and the change in sensitivity to pain cause the desired pain alleviation.
• Central reactions
The hierarchical centers of the CNS—brain stem, central gray matter, hypothalamus, thalamus, and cerebrum—compare and process the simultaneously arriving impulses created by acupuncture and disorder. This results in a centrally controlled impulse response. The brain stem controls the connection to vital functions like respiration and the adaptation of cardiac and circulatory regulation. The central gray matter primarily controls the production of endorphins, thus, pain alleviation. The hypothalamus directs the connection with functions of the autonomic nervous system and the engagement of the endocrine system. In the thalamus the emotional connection is added and transmitted to the cerebral cortex, here the psychological/physiological connection, awareness, takes place. This is where every occurrence (insertion of an acupuncture needle/disease symptom) receives its final interpretation.
That explains how a complex impulse pattern of nociceptors can be diminished, superseded, or intensified. In an accepted therapeutic situation, the same impulse that causes fear and panic due to pain can alleviate pain through descending inhibition with local, segmental, and global projection. In this situation, its effect is perceived as generally relaxing and pleasurable. The central neural reactions are supported by activation of the endocrine system through the hypothalamus. Hormones that are secreted at this location are called stress hormones. Stress hormones include the releasing hormones of the hypothalamus, pituitary hormones, ACTH, follicle-stimulating hormones (FSH), luteinizing hormones (LH), anti-diuretic hormones (ADH), prolactin, steroid hormones of the gonads (estrogens, androgens) and of the adrenal cortex (cortisone, aldosterone), and hormones of the adrenal medulla (epinephrine and norepinephrine). The long-term effects of the neuropeptides, endorphins and enkephalins, can explain the pain-reducing, sedating, and euphoria-inducing effects of acupuncture. These neuropeptides are produced in the hypothalamus and the central gray matter, but are also released in other parts of the CNS. They act as neuromodulators by connecting to receptors of the postsynaptic membrane where they diminish the response to secreted neurotransmitters (e. g., acetylcholine and dopamine).
Microinvasive acupuncture counteracts symptoms, activates the body’s mechanisms of counter-regulation, and, thus, reinstates homeostasis.
Integrating Acupuncture Into a Treatment Plan
Qualification
Acupuncture treatment should be modified to the conditions in the West. This adaptation needs to be made considering the elemental structures and rules of TCM. A prerequisite for successful application is comprehensive training.
A diligent clinical approach is part of each acupuncture therapy. This includes a thorough case history, a clinical examination, and, if necessary, the assistance of diagnostic aids, such as laboratory testing and machine-aided diagnosis, in order to find the correct Western diagnosis and the proper therapy. Only then can the therapist decide whether acupuncture is an alternative to Western approaches or a complementary therapy for each individual patient. After an in-depth consultation, the patient is able to consent to acupuncture treatment.
“Nihil nocere” (“Do not harm”) is the most important treatment rule. Acupuncture, as an invasive mode of treatment, has to be practiced according to Western safety standards. Strict compliance with safety procedures is required. Indiscriminate and unqualified use of acupuncture (“Let’s try it, it can’t hurt”) damages the image of this treatment method, endangers the patient, abuses the trust of the patient, and causes the patient to perceive the competence of the therapist as negative.
List of Requirements
The list of requirements includes the following mandatory conditions:
• Adequate acupuncture training and qualification of the therapist (for physicians a minimum of 140 hours, for midwifes 40 hours)
• Diagnosis based on well-founded medical criteria
• Acupuncture must be indicated (for established and important indications, see p. 88)
• Contraindications need to be ruled out.
The therapist should not try to persuade the patient to have acupuncture treatment. She has to agree and her circumstances have to favor acupuncture.
Only if these prerequisites are met should or may the therapist provide acupuncture treatment.
List of Safety Procedures
Due to the invasive nature of acupuncture, the therapist bears a particular responsibility for keeping risks to a minimum. He/she does so by strictly following the list of safety procedures.
It is important, for the success of the therapy, to establish a trusting relationship during all phases of acupuncture therapy, from the initial consultation to insertion of the first needle.
The patient is more likely to experience pain if she lacks confidence in the method or the therapist. When practicing acupuncture, the therapist should always project confidence and competence, even in the learning phase. Personal experience of this treatment method is mandatory before practicing acupuncture. Only personal experience allows the therapist to possess the necessary confidence in and assess possible reactions to acupuncture.
Indications For Acupuncture Therapy
Acupuncture therapy is not indicated in the case of malignant disease. According to the basic principle of regulatory therapy (“acupuncture can treat a disorder, but cannot repair what is damaged”), an effect of acupuncture on malignant conditions cannot be expected. Nevertheless, acupuncture can be a useful treatment for malignant cases by accompanying conventional medical therapy. It can, for example, alleviate nausea induced by chemotherapy, anxiety, restlessness, and insomnia. Acupuncture can also aid in pain management. Epilepsy does not constitute a contraindication for acupuncture.
Contraindications
Infants and children up to six years of age are usually not treated with needle acupuncture; laser acupuncture, moxibustion, or acupressure are an option. The elderly, whose responses have considerably slowed down, experience limited therapeutic effects. The appropriateness of this treatment mode needs to be considered with respect to this aspect.
Acupuncture is contraindicated in the case of psychiatric disorders, particularly endogenous psychoses if a person might harm themselves or others. In contrast, anxiety, tension, and restlessness are known to be indicated conditions for acupuncture.
If a patient has noticeable difficulties communicating (language issues), the use of acupuncture needs to be carefully considered. Undecided or fearful patients should never be talked into or even forced into acupuncture therapy. Before acupuncture treatment, each patient should be screened to find out whether acupuncture is a suitable therapy form for her. This requires her trust in the therapist and the method. If an extensive conversation does not create this trust, acupuncture should be avoided in this patient.
Characteristics of Acupuncture During Pregnancy
Traditionally, many acupuncture points are considered contraindicated during pregnancy (Table 22). It is an established fact that acupuncture does not have specific dangerous effects on pregnancy. Because acupuncture may reduce symptoms, an already latently impaired or endangered pregnancy with premature labor, or the onset of a miscarriage, or premature delivery might go unnoticed.
The traditional view and the prohibition of use of certain points during pregnancy is obsolete and not corroborated by our understanding of pathophysiology.
Table 22 Contraindicated points during pregnancy according to TCM
First month | Da du (SP-2), xing jian (LR-2) |
Second month | Yang ling quan (GB-34) |
Third month | Lao gong (PC-8) |
Fourth month | Yang chi (TB-4), tian jing (TB-10), nei guan (PC-6) |
Fifth month | Yin bao (LR-9) |
Sixth month | Feng long (ST-40), li dui (ST-45), shou san li (LI-10) |
Seventh month | Lie que (LU-7), shao shang (LU-11) |
Eighth month | Shang yang (LI-1), er jiang (LI-2), shou san li (LI-10), qu chi (LI-11) |
Ninth month | He gu (LI-4), yong quan (KI-1), ran gu (KI-2), fu liu (KI-7) |
General | Zu san li (ST-36), he gu (LI-4), san yin jiao (SP-6) |
The old lists of acupuncture points that are contraindicated during pregnancy and the apparently nonsensical differentiation of points according to the month of pregnancy can only be historically justified.
Complications
It is important to know about possible complications in order to avoid them and to make the right choices in case of an emergency. Fundamental complications can be avoided by obeying the safety procedures. Direct complications stem from the application of acupuncture correctly; indirect complications stem from improper application of the method.
Direct Complications
Bleeding and hematoma formation. Each time a needle is inserted, slight venous bleeding and, thus, formation of a hematoma is possible, particularly in the case of increased hemorrhagic diathesis. Light venous bleeding does not usually cause complications. After removing the needle, light compression at the point of insertion prevents hematoma formation (do not rub with a swab!). In some indicated cases, some bleeding after needle removal is therapeutically desirable (effect of cupping).
Infections. There is a chance that infections caused by bacteria, viruses, or other infectious microorganisms can be spread. Theoretically, acupuncture needles could transmit hepatitis or HIV. These risks can be eliminated almost entirely by adherence to asepsis and antisepsis. The use of sterilized disposable needles is the rule in acupuncture therapy today, mainly to eliminate the possibility of infection.
Orthostatic dysregulation. Patients with strong autonomic regulation and a vacuity condition tend to suffer from increased orthostatic dysregulation. This state may announce itself, shortly after needle insertion, through vertigo and pallor, particularly when needling a seated person. All needles have to be removed if the condition does not change after a brief moment. Putting the patient in supine position may prevent fainting. Subsequent acupuncture treatments on this client should only be performed in the supine position. In the later stage of a pregnancy, a side position instead of the supine position should prevent caval compression syndrome.
Severe pain (searing pain) that was caused by direct lesion of a pain receptor, nerve fiber, or nerve root has to be relieved.
This problem can be solved immediately through repeated manipulation or slight retraction of the needle.
Stuck needle. Once in a while, a needle cannot be removed immediately at the end of the acupuncture treatment. This may cause considerable discomfort to a patient and an inexperienced therapist. In reality, this phenomenon is caused by a change in posture, which affects tissue and muscle tension. When the original position is resumed and the area around the needle is lightly massaged, the needle can be removed with careful pulling and twisting motions. If the needle is still stuck, nothing should be done for a few minutes. This gives the tissue the opportunity for reflectory relaxation. In any case: Stay calm! If one obeys these rules, every needle can be removed without a problem after a short period of time.
Forgotten needles. These constitute a harmless complication that causes unnecessary flurry, particularly if the patient notices the needle after arriving home. It does happen that needles are overlooked, especially in body regions that are less accessible (e. g., very hairy areas). During each treatment, all chosen points should be documented in the case file. At the end of the treatment, the removed needles should be compared with the documentation.
Broken needle. Following the introduction of disposable needles, this complication has been relegated to the past. Previously in the West and in present-day China, this frequently occurring complication resulted from metal fatigue following sterilisation. The use of high-quality disposable needles has almost entirely eliminated this problem. Needles should never be completely inserted and should protrude above the surface. In the case of needle breakage, the needle can be removed with forceps.
Injury to sensitive structures. The use of acupuncture therapy requires special attention to sensitive regions and vital organs. Injury to the pleura leading to pneumothorax formation as well as injury to internal organs may technically occur. If the general rules of treatment, correct depth of insertion, and manipulation techniques are applied, this complication can also be almost entirely eliminated. In the case of potentially dangerous points, depth and direction of needle insertion should never exceed textbook recommendation, and the necessary manipulation should be executed with proper caution. It is common to apply electrostimulation if extended manipulation techniques are required. This prevents additional involuntary insertion of the needle. Also, the patient perceives electrostimulation as more pleasant than intense, repeated manipulation.
Sedation/fatigue. Frequently, during and after acupuncture treatment, patients become tired, which can result in a delayed response time. Patients may drive a vehicle following an outpatient acupuncture treatment after being warned accordingly.
Indirect Complications
Severe indirect complications may occur if acupuncture is not properly applied, or important requirements or contraindications are ignored:
• Missing an important surgical indication and its resulting consequences.
• Not recognizing a malignant disease and delaying the correct diagnosis, which may considerably worsen a client’s prognosis.
• Missing an acute critical condition that requires specific intervention (e. g., gestosis and preeclampsia, early labor, etc.).
• Ignoring the possibility of being a danger to oneself or others in the case of psychological disorders or addicts.
• Not being aware of the legal consequences if the therapy is not applied with proper knowledge or by unqualified persons.
Complications have to be expected if novel stimulation techniques are used in addition to the traditional needle acupuncture. If, for example, the axis of the heart is crossed using electrostimulation, cardiac arrhythmia may occur. Pre-existing heart damage requires particular attention to this risk.
Electrostimulation at PC-6 must always be performed with caution. Electrostimulation also carries the risk of disrupting the function of some pacemakers, and also provoking a fit in epileptic patients. However, acupuncture usually increases the stimulus threshold and, thus, reduces the risk of epileptic seizures; in China, seizure disorders are considered an indication for acupuncture.
Laser acupuncture also involves certain risks. Even though only low-energy lasers, so-called soft lasers, are used and allowed in acupuncture therapy, the retina may be damaged by a direct ray. According to the latest medical equipment code (MedGV in Germany), all persons present during a laser treatment have to wear laser safety glasses.
 General Recommendations
General Recommendations
In order to minimize the risk of infection, recommendations include:
• Always use disposable needles.
• Disinfect soiled areas of the skin.
• In case of patients with decreased immunity or diabetes mellitus, disinfect the point locations before inserting the needles (body acupuncture does not usually require disinfection).
• Inform patients about the signs of infection before using permanent needles.
Needling sensitive patients (vacuity patients) in a supine position can prevent orthostatic dysregulation or shock. In the case of shock, all needles must be removed immediately and the patient placed in a supine position (legs elevated if necessary). Emergency points such as PC-9 and GV-26 can be applied.
Proper technique avoids pain during needle insertion (quick piercing of the skin). Repeated light manipulation or slight retraction of the needle can alleviate pain that occurs upon insertion of the needle. A small drop of blood following the removal of needles is insignificant. Hematoma formation can be avoided through light compression using a swab at the point of needle insertion. In the case of repletion conditions, light bleeding after removal of the needles is desirable.
A therapeutic aggravation (Erstverschlimmerung) is common to all regulative therapies. The patient must be warned that this may occur following acupuncture treatment of certain diseases.



