Hormonal contraception takes four forms:
COMBINED PILL
Mode of action
HORMONAL CONTRACEPTION
Constituents
Choice of pill
Major side-effects
Thrombo-embolism
Myocardial infarction and stroke
Hypertension
HORMONAL CONTRACEPTION
Contraindications
Contraindications
Special precautions
History of cardiovascular disease
Collagen diseases
Hypertension
Otosclerosis
Heavy smoking
Diabetes mellitus
Obesity
Sickle cell disease
Migraine
Surgical operations
Chronic hepatitis
Severe varicose veins
Breast cancer
History of depression
Endogenous depression.
Age over 35.
Cancer and the pill
Failure of the pill
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Contraception
1. Combined (oestrogen/progestogen) pill.
2. Progestogen-only pill.
3. Progestogen-only injections or implant.
4. Progestogen intra-uterine system.
This is by far the commonest form of oral contraception (OC). About 3 million women in the United Kingdom are said to be ‘taking the pill’. It is the most effective form of contraception apart from sterilisation and, for many women, the most acceptable aesthetically. The pill is taken daily for 21 or 28 days depending on the formulation, and a withdrawal bleed will normally occur in the pill-free days or during the 7 placebo days of the everyday preparations.
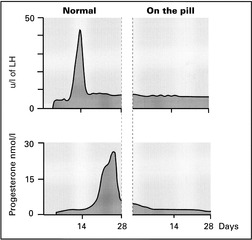
(a) The pill prevents ovulation. FSH secretion is depressed so that normal follicular development does not occur and the LH peak is abolished. This is mainly due to oestrogen but progestogens can also suppress ovulation, at least in large doses.
(b) The endometrium does not develop normally and the absence of a corpus luteum prevents the preparation of an endometrium suitable for implantation. There is a ‘pseudo-atrophy’ so that, even if ovulation occurs, implantation is unlikely. This is a combined effect of oestrogen and progestogen.
(c) Changes in cervical mucus make sperm penetration less likely. This is a progestogen effect.
Most pills are monophasic, i.e. contain the same amount of oestrogen and progestogen throughout the cycle. There are, however, biphasic and triphasic pills which aim to mimic the normal cyclical variation in hormone levels. Unopposed oestrogen is not given at any time however.
A large number of different combined preparations are available. The aim is to find, for the individual patient, the preparation with the lowest oestrogen and progestogen content which gives good cycle control and minimal side-effects.
Usually a standard strength preparation (30 or 35 micrograms of oestrogen) combined with etynodiol, levonorgestrel or norethisterone will be prescribed. The newer progestogens desogestrel, gestodene and norgestimate appear to have less adverse effects on blood lipids but, in the case of desogestrel and gestodene, have also been associated with an increased risk of venous thromboembolism. Combined preparations containing these agents, therefore, should only be used by women who are intolerant of other combined oral contraceptives and are prepared to accept an increased risk of thrombo-embolism.
Low-strength preparations (containing 20 micrograms of oestrogen) may be suitable for obese or older women provided there is no other contraindication to a combined oral contraceptive.
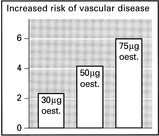
High-strength preparations (containing 50 micrograms of oestrogen) provide greater contraceptive security but with an increase in the possibility of side-effects.
The phasic pills have the lowest total dose of steroid and may also, therefore, be preferred for older women.
This appears to be due mainly to the alteration in clotting factors due to the oestrogen component and is dose-related, hence the introduction of low-dose oestrogen or progestogen-only pills. Even the low-oestrogen pills are associated with a significantly higher risk in women over 35, and hypertension and obesity are predisposing factors.
The excess risk with oral contraceptives containing levonorgestrel, norethisterone or ethnodiol is around 5 to 10 cases per hundred thousand women per annum. Recent studies suggest that combined oral contraceptives containing desogestrel and gestodene are associated with a two-fold increase in this risk, compared with those containing other progestogens. It was this information that led the Committee on Safety of Medicines in the UK to issue the advice noted above on the prescribing of preparations containing desogestrel and gestodene.
Oral contraceptive users, especially women over 35 who smoke, run an increased risk of these diseases. Arterial disease is attributed mainly to the effects of the progestogens. Progestogens have been shown to lower the level of high-density lipoprotein 2 (HDL2), the level of which is inversely proportional to the risk of heart disease: high concentrations of HDL2 give a lower risk of heart disease. The newer progestogens, desogestrel and gestodene, did not lower HDL2 to the same extent and were thus expected to reduce the risk of stroke and myocardial infarction in pill users.
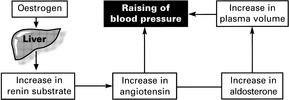
OCs gradually raise the blood pressure, sometimes to the hypertensive range. The blood volume is increased by fluid retention, and the secretion of angiotensin is increased.
Below are listed the commonly accepted contraindications to the pill and the circumstances in which special precautions should be taken. It must be remembered, however, that few of these contraindications are absolute and the risks of the patient using the pill have to be set against the possibly increased risk of pregnancy if an alternative method is employed. Absolute contraindications are cardiovascular disease, liver disease and breast cancer.
Progesterone stimulates mitotic activity in breast endothelium, and evidence has been published which suggests that long-term oral contraceptive users before age 25, especially with the more potent progestogens, may incur an increased risk of subsequent breast cancer.
Long-term use of the oral contraceptive is associated with a slight increase in rates of cervical cancer and intra-epithelial neoplasia. Long-term users should certainly have regular cervical cytology undertaken.
Prolonged oral contraceptive use depresses mitotic activity in the endometrium and follicular maturation in the ovary, and these effects are considered to offer some protection against cancer of these tissues.
The failure rate of the combined pill is very small, between 0 and 1%, and there is often an avoidable factor.
1. If a pill is missed it should be taken when remembered, and the next pill is taken at the usual time. Additional precautions should be used for the next 7 days.
2. Vomiting or diarrhoea may impair absorption.
3. Certain groups of drugs such as the anticonvulsants phenytoin, carbamazepine and phenobarbital and the antibiotic rifampicin are known to increase the metabolic activity of hepatic enzymes, and increase the rate of excretion of contraceptive steroids. (Compare the treatment of neonatal jaundice with phenobarbital.)