Chapter 19 Congenital Anomalies and Benign Conditions of the Uterine Corpus and Cervix
 Congenital Anomalies of the Uterine Corpus and Cervix
Congenital Anomalies of the Uterine Corpus and Cervix
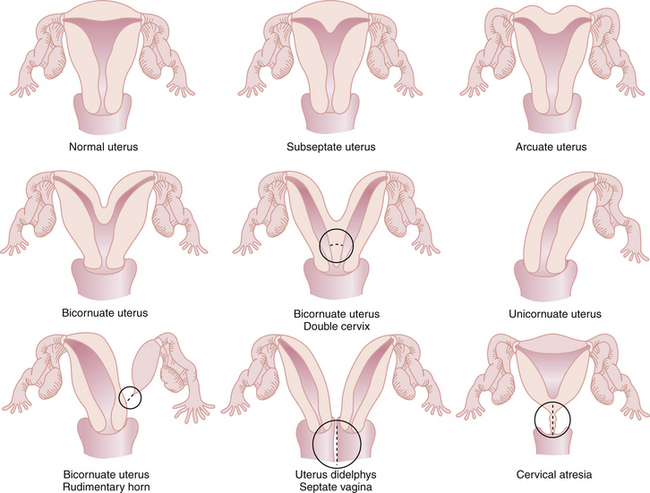
The most common anomalies of the uterus result from either incomplete fusion of the paramesonephric ducts, incomplete dissolution of the midline fusion of those ducts, or formation failures. Figure 19-1 shows variations of uterine and cervical development and demonstrates that communication between the dual systems can exist at several levels. Failure of fusion is most evident in uterus didelphys, which presents with two separate uterine bodies, each with its own cervix and attached fallopian tube and vagina. A bicornuate uterus with a rudimentary horn also represents a fusion failure. Less complete fusion failure is seen in the bicornuate uterus with or without double cervices. Incomplete dissolution of the midline fusion of the paramesonephrica explains the septate uterus. Failure of formation can be seen in the unicornuate uterus. In müllerian agenesis, there is complete lack of development of the paramesonephric system. The affected woman generally has incomplete development of the fallopian tubes associated with the absence of the uterus and most of the vagina. All these conditions occur in normal karyotypic and phenotypic females but can be associated with important anomalies of the urinary system such as a horseshoe or pelvic kidney.
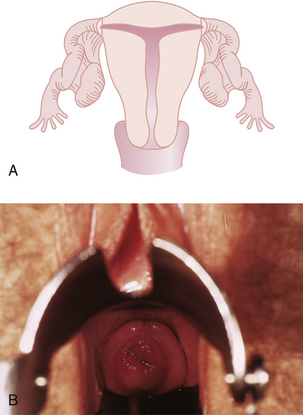
Although all these anomalies can occur spontaneously, they may also be caused by early maternal exposure to certain drugs. The most notable of these drugs is diethylstilbestrol (DES). A DES-exposed female infant has an increased risk for a small, T-shaped endometrial cavity (Figure 19-2A) or cervical collar deformity (Figure 19-2B). DES exposure in utero can also produce fallopian tube abnormalities, although it does not appear to cause abnormalities of the urinary tract.
 Benign Neoplastic Conditions
Benign Neoplastic Conditions
UTERINE LEIOMYOMAS
Characteristics of Leiomyomas
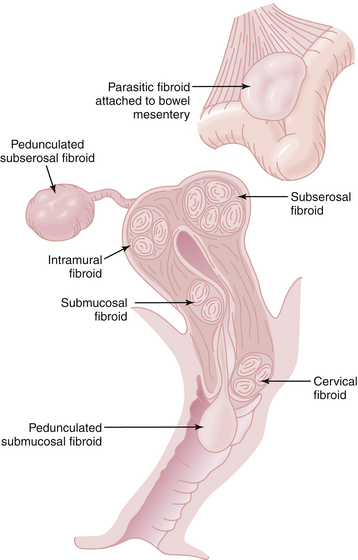
Leiomyomas always arise within the myometrium (intramural), but some migrate toward the serosal surface (subserosal) or toward the endometrium (submucosal), as depicted in Figure 19-3. Individual tumors may migrate further when they develop large pedicles. The submucosal leiomyomas can extend through the endometrial canal and abort from the cervical os. An aborting leiomyoma causes significant bleeding and cramping pain. A subserosal leiomyoma on a long pedicle can present as a mass that feels separate from the uterus. Rarely, pedunculated subserosal myomas attach to the blood supply of the omentum or bowel mesentery and lose their uterine connections to become parasitic leiomyomas. Leiomyomas can also arise in the cervix, between the leaves of the broad ligament (intraligamentous), and in the various supporting ligaments (round or uterosacral) of the uterus. Leiomyomas can invade and fill the vena cava retrograde up to the level of the atrium (intravenous leiomyomatosis).