COLON
What is the best next step in the management of this patient?
a. Complete blood count (CBC)
b. Stool occult blood
c. Iron studies
d. Basic metabolic profile
e. Colonoscopy
f. All of the above
Answer f. All of the above
This patient is presenting with signs and symptoms of anemia, and given his age and risk factors most likely has colon adenocarcinoma. The first step is to establish the patient’s cause of fatigue by checking his CBC, iron studies, and kidney function. This should be combined with a stool occult blood test and eventually a colonoscopy if possible. If the patient had presented with melena, an upper endoscopy would have been considered, but given the change in bowel habits and stool caliber, it is likely a left-sided malignancy.
Hematochezia is more often caused by rectosigmoid than right-sided colon cancer.
Given the patient’s family history, when would have been the appropriate screening interval for this patient?
a. Age 40 years and every 5 years thereafter
b. Age 40 years and every 10 years thereafter
c. Age 45 years and every 5 years thereafter
d. Age 45 years and every 10 years thereafter
e. Age 50 years
Answer a. Age 40 years and every 5 years thereafter
The screening interval is normally age 50 years and every 10 years thereafter, if normal, for all patients without a family history. However, in patients who have a first-degree relative with colon cancer, the screening should begin 10 years before the age of the relative or age 40 years, whichever comes first, and should be repeated every 5 years.
Gene changes in colon cancer
• General colon cancer: K-ras mutations
• Familial adenomatous polyposis: APC gene
• Hereditary nonpolyposis colon cancer syndrome or Lynch syndrome: MSH2, MLH1, and PMS2 genes
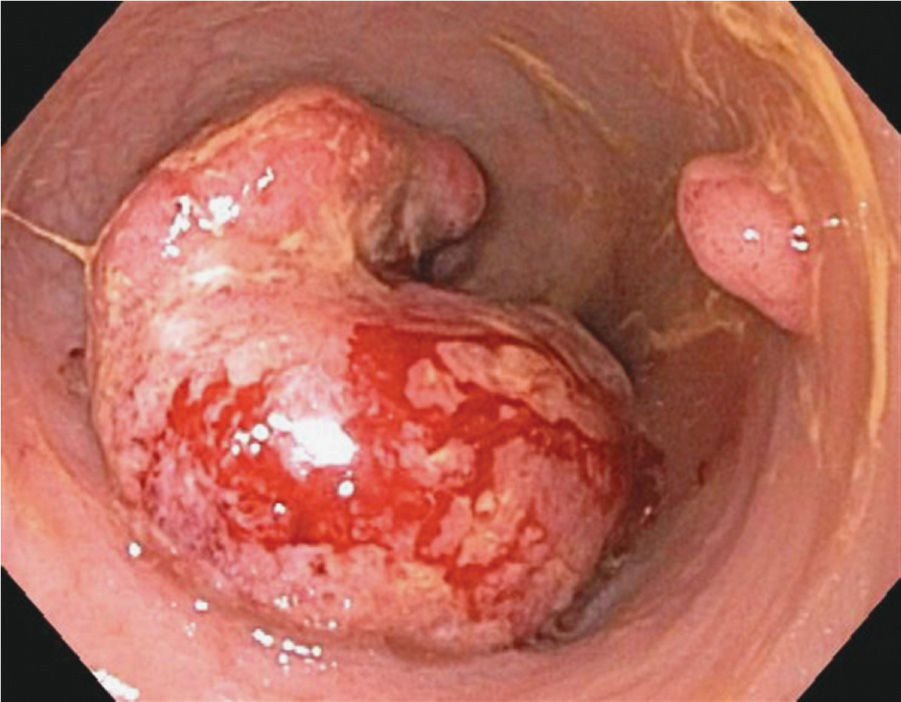
Figure 9-1. Colon cancer. (Reproduced, with permission, Greenberger NJ, Blumberg RS, Burakoff R, eds. Current Diagnosis & Treatment: Gastroenterology, Hepatology, & Endoscopy. 2nd ed. New York: McGraw-Hill; 2012.)
In iron deficiency anemia, iron studies will reveal low serum iron, low serum ferritin, and TIBC.
What is the best next step in the management of this patient?
a. Computed tomography (CT) scan of the chest, abdomen, and pelvis
b. Surgical resection
c. Chemotherapy with a 5-fluorouracil (F-FU)–based regiment
d. All of the above
Answer a. Computed tomography (CT) scan of the chest, abdomen, and pelvis
Before the establishment of a treatment regimen, staging of the colorectal cancer is needed because the stage changes the management plan. Surgical resection combined with chemotherapy is considered to be a part of treatment after a patient has the staging established.
5-FU is a thymidylate synthase inhibitor that in turn causes synthesis of the pyrimidine thymidine to be blocked.
What is the most likely diagnosis?
a. Gastroenteritis
b. Ulcerative colitis
c. Toxic megacolon
d. Ischemic colitis
e. Diverticulitis
Answer c. Toxic megacolon
Patients presenting with severe abdominal distension, dehydration, pain, and fever with diarrhea are likely to have toxic megacolon. There are numerous causes, but this patient’s is Clostridium difficile infection caused by recent antibiotic exposure. Gastroenteritis does present with nausea, vomiting, and diarrhea but is not associated with severe distension and pain. Ulcerative colitis does not present this acutely and would have bloody diarrhea. Ischemic colitis and diverticulitis do not affect a patient this young and would not have a history of antibiotic exposure.
C. difficile is the leading cause of hospital-acquired diarrhea.
The BI/NAP1 strain of C. difficile is the most strongly associated with toxic megacolon.
What is the best next step in the management of this patient?
a. Abdominal radiography
b. C. difficile toxin assay
c. Intravenous (IV) normal saline
d. Complete blood count (CBC)
e. Basic metabolic profile (BMP)
f. All of the above
Answer f. All of the above
In a patient presenting with signs and symptoms of toxic megacolon, the initial management consists of obtaining an abdominal radiography, CBC, C. difficile toxin assay, and resuscitation of the patient with normal saline. A BMP is needed to ensure the patient does not have life-threatening electrolyte imbalances such as hypokalemia and to measure renal function. An abdominal radiography is the best initial test and is used to measure the dilation of the transverse colon, which is most commonly dilated. Dilation of 6 cm or more of is diagnostic of toxic megacolon.
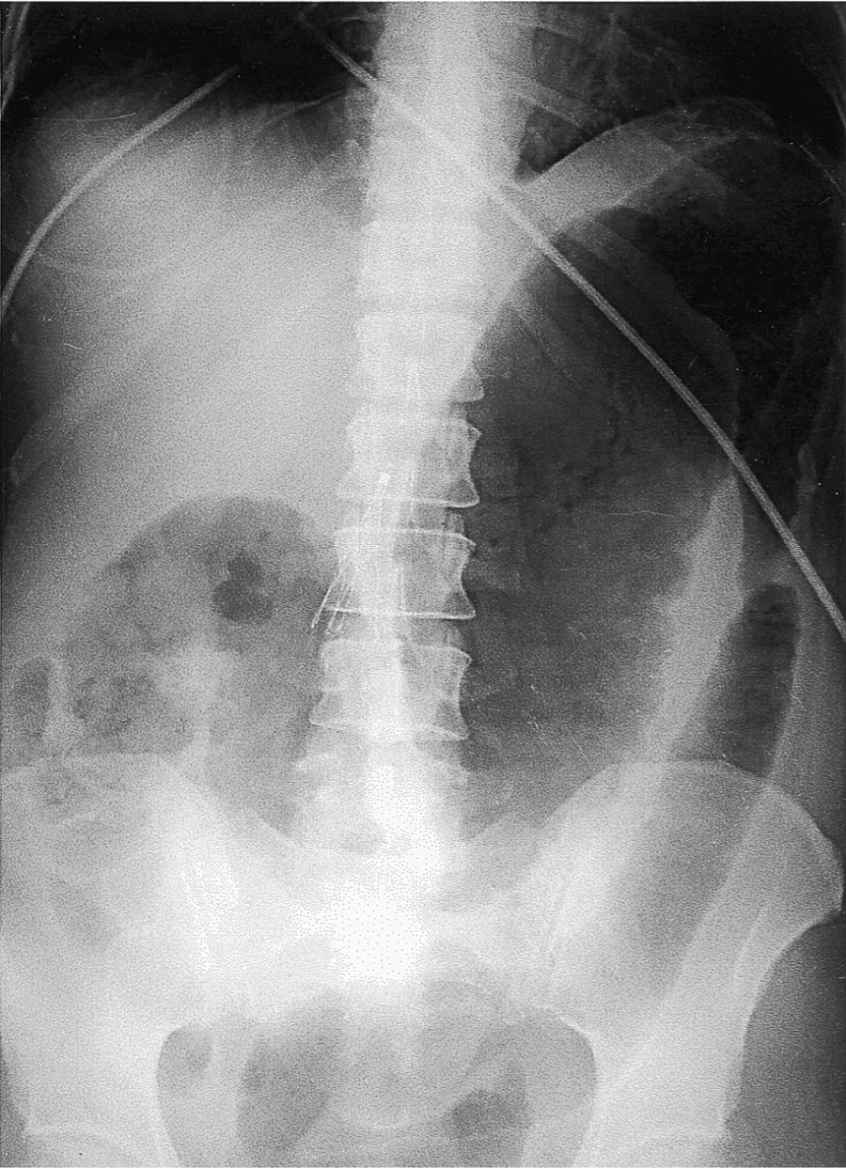
Figure 9-2. Toxic megacolon with perforation. Supine radiograph demonstrates marked mucosal nodularity and thickening of the transverse colon. (Reproduced, with permission, from Bongard FS, et al. Current Diagnosis & Treatment: Critical Care. 3rd ed. New York: McGraw-Hill; 2008.)
What is the most appropriate therapy for this patient?
a. Surgical consult
b. IV vancomycin
c. Oral vancomycin
d. Oral metronidazole
e. Rectal steroid suppository
f. Oral vancomycin and oral metronidazole
Answer f. Oral vancomycin and oral metronidazole
In patients with toxic megacolon caused by severe C. difficile colitis, the first step is to stop the offending antibiotic, then treat with vancomycin and metronidazole orally. Surgical consult is reserved for patients after 48 to 72 hours of observation under antibiotic therapy. IV vancomycin is always the incorrect answer in the treatment of C. difficile because it does not cross into the bowel from intravascular circulation. Surgery in the form of colectomy is for patients who do not improve within 48 to 72 hours or in those who show evidence of localized perforation.



