Fig. 12.1
Long term survival of osteosarcoma (a) and Ewing’s sarcoma patients (b) treated at our institution. Percentage of DFS at 15 years is 72 % for osteosarcoma patients and 68 % for Ewing’s sarcoma patients
12.2 Histological Study of Margins
Previous studies by our team indicate that invasion of the epiphysis by a tumor seems to be a question of time: there is a hypervascularization reaction which leads to an early ossification of the growth plate, and after that the tumor transgresses the physis. However, for epiphysiolysis to be indicated, the tumor must not have crossed the physis. For the series of patients reported here, imaging methods accurately revealed whether or not the physis had been involved by the tumor.
Histological examination of resected pieces confirmed in all cases that the tumor had not involved the growth plate. We used Indian ink staining to study the physeal margin of resection, where – because at the rate of distraction employed (1 mm/day) the growth plate is disrupted at the degenerative layer of cells – there is a thin layer of growth plate cells covering the bone (Fig. 12.2). Note that the 1 mm/day rate of distraction results in most of the growth plate being retained with the epiphysis.
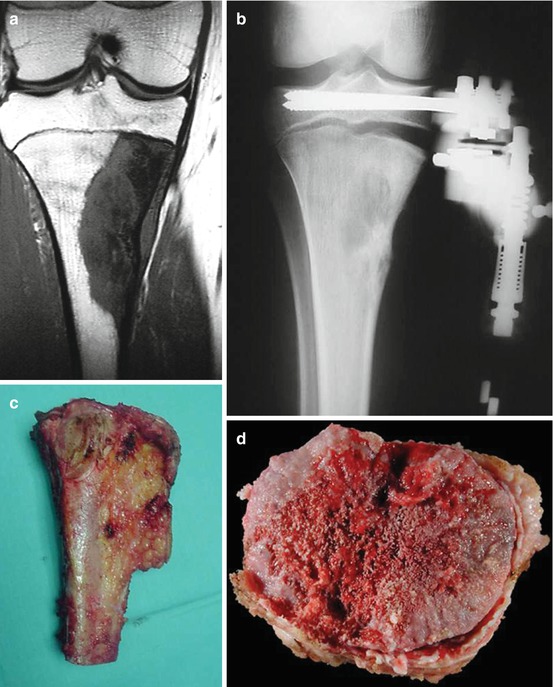

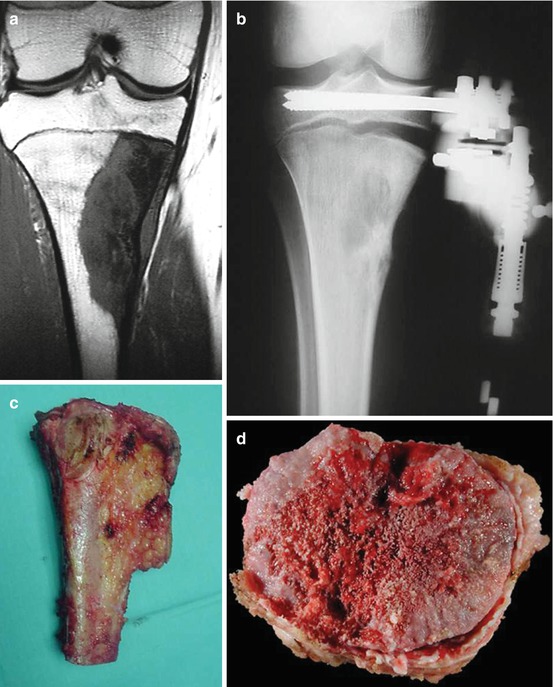

Fig. 12.2
Proximal tibia osteosarcoma apparently in contact with the growth plate. (a) After epiphysiolysis (b). This is, by definition, a wide margin (that is, there is no reactive tissue) (c–f)
12.3 Limb Function (Videos 12.1 and 12.2)
In most patients, preservation of the epiphysis has resulted in an excellent functional outcome. In addition, the long-term complications of joint substitution are avoided [3–5, 29–31] (Figs. 12.2, 12.3, 12.4, 12.5, and 12.6). The rates and natures of complications due to reconstruction procedures are similar to those encountered with other limb salvage techniques.
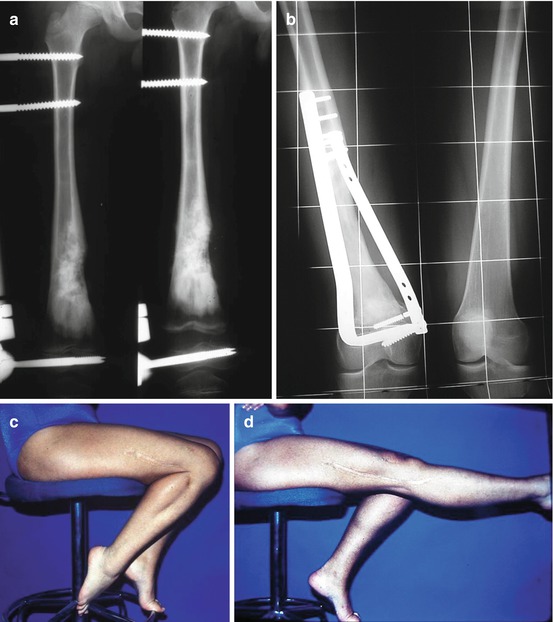

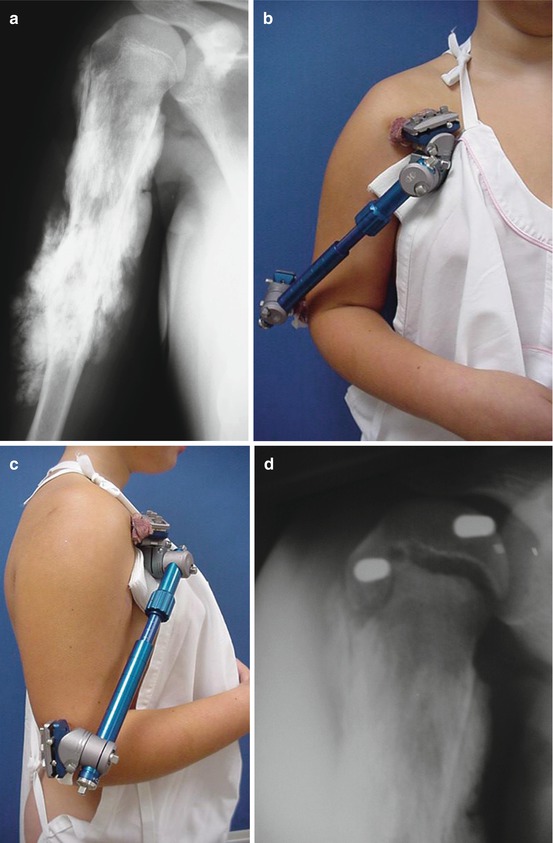
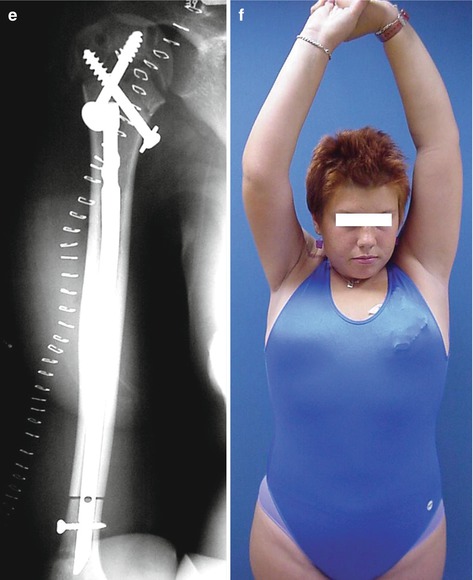

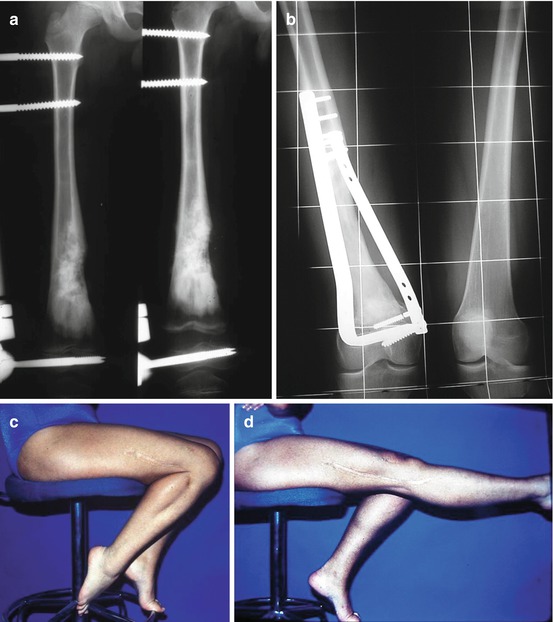
Fig. 12.3
(a) Physeal distraction in a metaphyseal osteosarcoma of the femur. (b) The reconstruction was carried out with autografts from the tibia and iliac crests. Twenty-three years after operation, the joint (b) and the functional results (c, d) remain excellent

Fig. 12.4
(a) Ewing’s sarcoma in the proximal metaphysis of the tibia. Physeal distraction was performed. (b) The reconstruction was carried out with an intercalary allograft. (c, d) Functional result
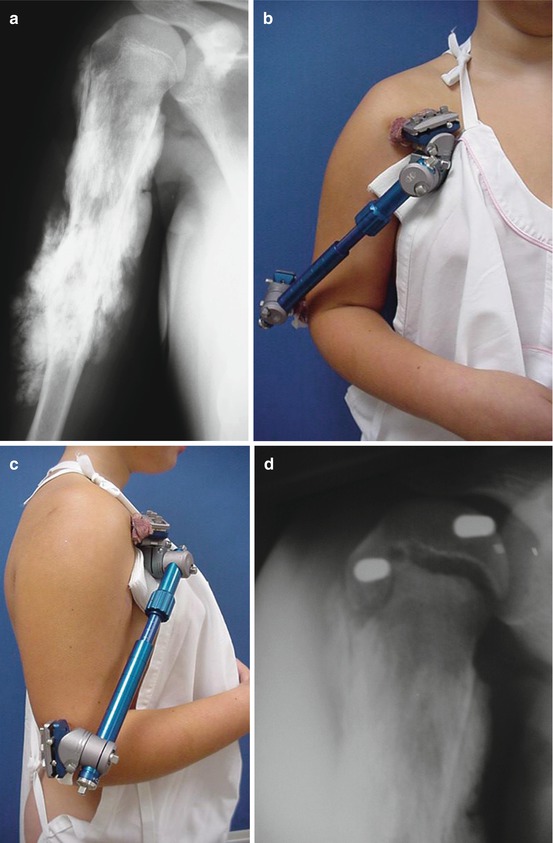
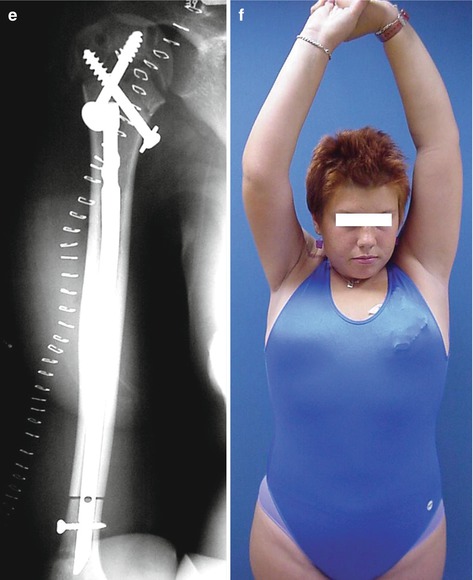
Fig. 12.5
(a–c) In the proximal humerus, due to the particular morphology of this growth plate, the pins should be placed anteriorly in the humeral head (see also Fig. 7.7), and posteriolaterally in the distal part, in order to avoid radial nerve damage. (d) After distraction, reconstruction was carried out (e) with an allograft. (f) Because it was possible to preserve the joint, the attachment of the rotator cuff and the axillary nerve, abduction of the shoulder is almost complete

Fig. 12.6
(a) Osteoarticular allograft for reconstruction of the shoulder after resection of a Ewing’s sarcoma in the proximal humerus. When the joint cannot be preserved, abduction of the shoulder, both active (b) and passive (c), is poor
12.4 Complications
12.4.1 Infection
This occurred in 7 % of patients, and therefore we conclude that the risk of infection is the same as in other limb salvage procedures. The risk is not higher because the external fixator is placed for only 10–15 days (Fig. 12.7). Most infections occurred after secondary operations performed in response to some other complication, such as, non-union or fracture of the graft. Therefore, in our series, infections were not related to the external fixator.


Fig. 12.7
(a) The risk of infection is not higher because the external fixator is only in place for 10–15 days. (b) In this case, one pin tract was removed in the surgical approach
Of the cases with infection, some were cured by systemic antibiotic therapy, but most required removal of an allograft, reattachment of the external fixator, insertion of gentamicin-impregnated cement, systemic antibiotic therapy [8], and, after elimination of the infection, implantation of a new allograft. The risk of infection is higher in allografts in comparison to autografts. This is another reason for choosing autografts for reconstruction in young children or after resection of small tumors.
12.4.2 Non-union of the Graft
About 14 % of patients required a further operation, with the addition of autologous grafts, to achieve union between the allograft and the host bone. Healing was achieved in all but one case.
12.4.3 Other Complications
As with other tumoral resection procedures, peroneal nerve palsy can occur; the neurotoxicity of chemotherapy is also involved in this palsy. Another complication is fracture of the united allograft, which can usually be successfully treated by osteosynthesis with a plate and screws and autologous graft.
Despite the number of complications, the results of intercalary reconstructions are better than those from other kinds of limb salvage surgery in growing children. The results published for old models of expandable prosthesis are generally poor. For example, recently, Manfrini et al. [15] reported that nine out of ten expandable prostheses required revision surgery (in some cases even twice) before the end of growth. The high price of expandable prostheses is another important factor to take into account. Nowadays, however, results are improving as new models are developed (see Chap. 3).
12.5 Incorporation of Graft
Before 1986, as we did not have a bone bank, we used autografts from the ipsilateral or contralateral tibia, and iliac crests (Fig. 12.8). Since 1986, for most patients with big tumors [32–34], we have used allografts [25].
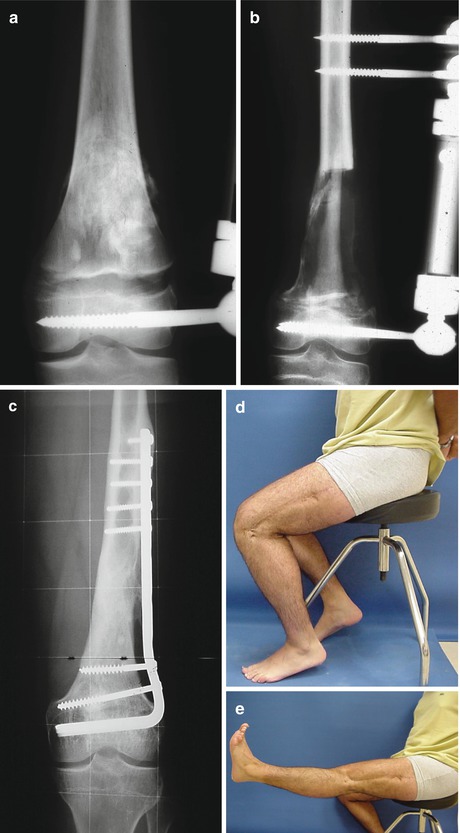
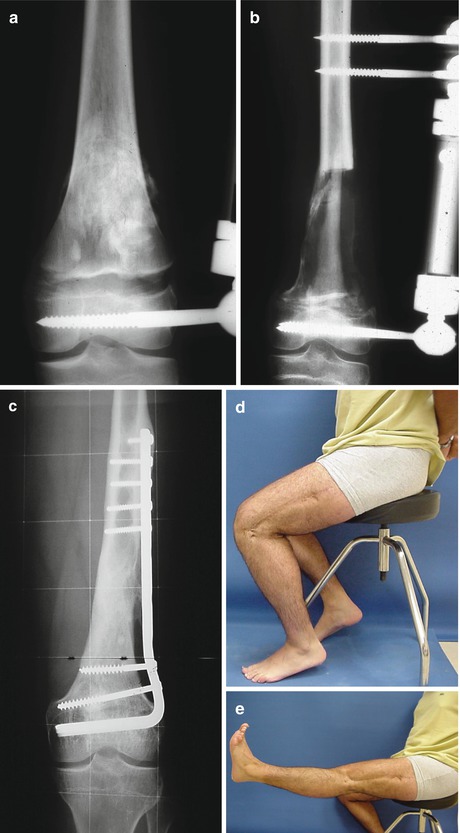
Fig. 12.8
(a) Radiograph showing an osteosarcoma of the femur in a 14-year-old boy after physeal distraction. (b) After resection of the tumor and autografting from the left tibia. The same frame was used for stabilizing the graft. (c) Twenty-two years later, the knee joint has an excellent aspect. (d, e) The function of the knee remains excellent. This patient plays sports without restrictions
The use of autografts resulted in an average of 2.8 operations per patient before graft consolidation [6, 40]. With allografts this average was reduced to 0.74, but it should be noted that patients were affected by other complications.
Consolidation at the metaphysis generally occurred before 6 months had elapsed, but at the diaphyseal end it often took longer than a year. In metaphyseal unions we used several types of osteosynthesis devices, such as, Kirschner wires, Enders, screws, and staples. Diaphyseal osteotomy and osteosynthesis devices are discussed at the end of this chapter.
Since 1987, at the Clínica Universidad de Navarra, we have used more than 1000 massive bone allografts in the conservative treatment of malignant bone tumors. The allograft type used depended on how the cartilage growth plate was affected and on the possibilities of preserving the joint near the tumor.
Monthly radiological follow-ups were carried out during the first year of systemic chemotherapy, with diagnostic studies to assess the local and systemic control of disease. Afterwards, follow-ups were every 3 months for another year, and subsequently every 6 months. In all cases, chemotherapy and radiotherapy were in accordance with the hospital’s cancer protocol [36] for the type of tumor.
12.5.1 Radiological Study
We used the ISOLS criteria (Table 12.1) to evaluate consolidation results [20] and analyzed the following factors which can influence consolidation: host and donor age, allograft length and location, osteotomy and osteosynthesis type, intra-arterial and systemic chemotherapy, and intraoperative and external radiotherapy. We performed a multi-variant statistical analysis with StatView software.
Table 12.1
ISOLS criteria regarding fusion of allografts
Excellent: Fusion complete. Osteotomy line not visible |
Good: Fusion >75 %. Osteotomy line still visible |
Fair: Fusion 25–75 % |
Poor: Fusion <25 %. No evidence of callus |
The mean consolidation time of metaphyseal osteotomies (including those cases in which physeal distraction was used before excision of the tumor) was 6.5 months; none of the factors studied had a statistically significant influence on consolidation. In metaphyseal osteotomies consolidation was achieved with minimal osteosynthesis (Fig. 12.9).

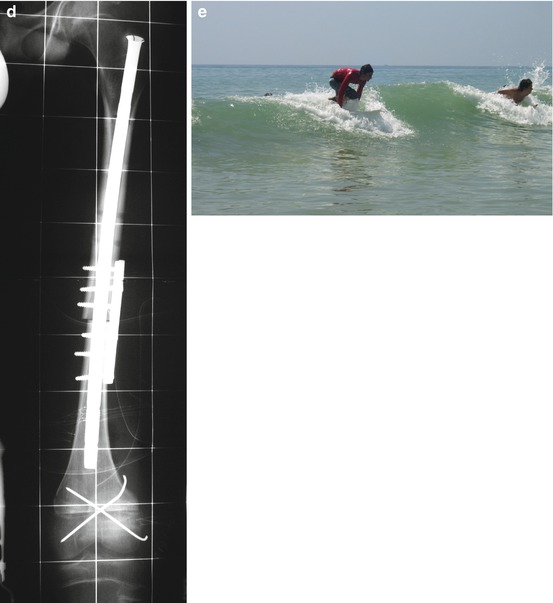

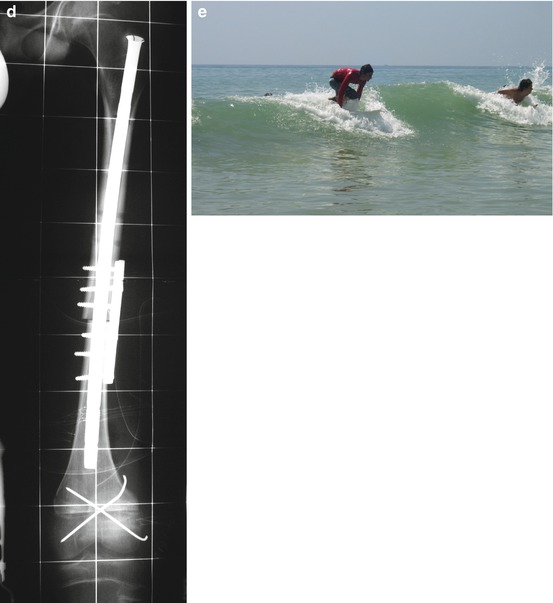
Fig. 12.9
(a, b) Osteosarcoma in the distal metaphysis of the femur of a 14-year-old boy. (c) Physeal distraction was performed and (d) an intercalary allograft was used for reconstruction. The healing at the distal junction was achieved with two Kirschner wires, while the diaphyseal junction required stronger osteosynthesis. (e) The same patient surfing
The mean consolidation time of diaphyseal osteotomies was 16 months (Fig. 12.10). We found no statistically significant differences in consolidation with the use of intra-arterial chemotherapy, intraoperative radiotherapy, donor age, osteosynthesis type (plates vs. intramedullary devices), osteotomy type (horizontal vs. oblique), type of tumor, or location of the tumor.
Fig. 12.10
Excellent fusion in a diaphyseal allograft-host bone junction
The mean consolidation time of metaphyseal osteotomies (6.5 months) is similar to that reported by others [16, 39]. Systemic chemotherapy delayed consolidation and this finding is supported by clinical data from other series [9–11, 17, 37, 38]. Experimental studies [14, 42] have also demonstrated that chemotherapeutic agents impair bone healing, and that allogeneic cortical bone grafts incorporate more slowly when chemotherapy is administered. External radiation also delayed consolidation. Radiation damages small and medium-sized blood vessels that supply nutrients to the bone, making it more difficult for the irradiated bone to heal [12]. Bone growth retardation resulting from irradiation is clearly a dose-dependent phenomenon [2, 13, 22, 41]. We believe that if the fracture of an allograft can heal with a standard treatment for fractures, it is because the allograft is revascularized at the time of the fracture [24].
12.5.2 Isotopic Study
In 36 patients a prospective isotopic study was performed [27] with 99mTc MDP in order to evaluate the revascularization of allografts. Bone scintigraphy with 99mTc HDP was performed 3 h after injection. Anterior and posterior views over both limbs were evaluated qualitatively by two physicians. Semi-quantitative measurements were performed with a region of interest (ROI) technique. Labeling was scored by location: over the bone allograft (A1); over the area just above the allograft (A2); as A1 but in opposite limb (A3); as (A2) but in opposite limb (A4). Background over soft tissues was considered and subtracted from all the ROIs. The allograft uptake was related with the uptake over A2 and A3, and two indices were obtained: I1 = A1/A2 and I2 = A1/A3. A further index, A2/A4, was also calculated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


