chapter 21 Clinical Evaluation for Possible Child Abuse
Obtaining the History
Physical Examination
Documentation
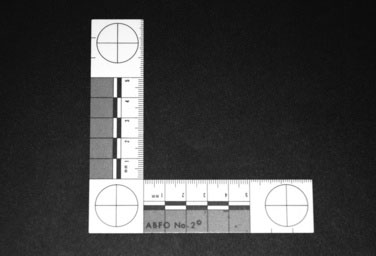
3. A ruler, preferably one approved by the American Board of Forensic Odontologists (ABFO) (Fig. 21–1). These display a circle upon their surface, to allow for adequate assessment of picture distortion as a result of the angle at which the picture was taken. Alternatively, you can use a measuring tape.
4. A color chart (Fig. 21–2) to allow for assessment of the color quality of the image. (See the color version on Student Consult).
5. A detailed body map showing anterior, posterior, medial, and lateral surfaces of all areas of the body (Fig. 21–3 and a full-page version on Student Consult).
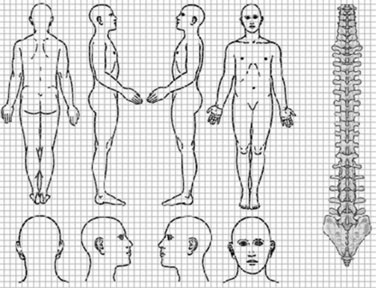
FIGURE 21–3 A sample body map.
(Modified from http://www.pain-initiative.com/e1833/e5688/e5887/diagram_eng.gif)
Obtaining Pertinent History
Formulating questions for history of present illness
| Child: | “He hurt my noonoo.” |
| Physician: | “Hmmm, I’m not sure I know exactly what you mean when you say noonoo, do you know another word for it?” |
| Child: | “You know, my privates!” |
| Physician: | “Oh, I see. Just to be sure I’m thinking of the right privates, “Can you show me where your noonoo is?” |
| Child: | “There, silly!” |
| Child: | “He put his stick in my bird.” |
| Physician: | “Do you mean his penis?” |
| Child: | “Yes.” |
| Physician: | “Is your bird your vagina?” |
| Child: | “Uh-huh” |
| Physician: | “Did it hurt?” |
| Child: | “Yeah.” |
| Physician: | “Did he put it in your mouth?” |
| Child: | “Yes.” |
| Physician: | “How about your bum?” |
| Child: | “He put his stick in my mouth.” |
| Physician: | “In your mouth?” |
| Child: | “Yeah and sometimes my bird too.” |
| Physician: | “Hmmm. What’s that like?” |
| Child: | “Kinda funny ’cause it gets all big and it stands up.” |
| Physician: | “And how does that feel when that happens?” |
| Child: | “Goodish badish.” |
| Physician: | “Really… anything else?” |
| Child: | “Kinda wet and goopy too.” |
| Physician: | “I see…” |
| Child: | “But that’s okay—we use Kleenex on the night table to clean up.” |
Physical Examination
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree