chapter 16 Clinical Endocrine Evaluation
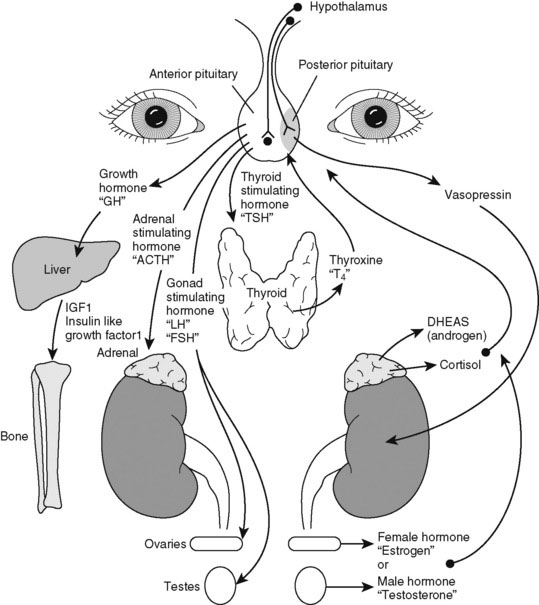
Pediatric endocrinology has special appeal because most childhood endocrine disorders are treatable. A specific diagnosis is usually possible on clinical grounds alone. Do not be intimidated by the myriad of hormone assays and endocrine tests needed to evaluate excesses or deficiencies. We have neatly arranged them all in an interrelated hormone map, which shows the feedback control of hormone action (Fig. 16–1). A good practice is to draw such a picture as you are explaining the details of hormone action to the family. Doing so slows down your explanation and makes you translate the medical lingo while still providing the correct names for hormones.
Approach to the Physical Examination of a Child with Possible Growth Hormone Deficiency
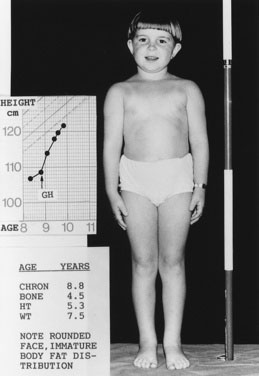
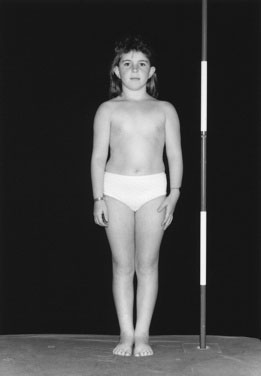
Children with GHD are described as cherubic (Figs. 16-2 through 16-4). They appear younger than their chronologic age, having a rounded face, chubby limbs, and “puddling” (or dimpling) of the anterior abdominal fat. Because of their infantile appearance, further enhanced by a high-pitched reedy voice, adults may baby them or classmates may carry them around like the class pet.
Height and weight percentiles (see Fig. 3–4) are usually discrepant in GHD, with a high weight-to-height ratio. This is a major clue to the need for detailed endocrine investigation. Chronic disease, especially inflammatory bowel disease, may be quite silent and manifest as short stature but, by contrast, with a low weight-to-height ratio.
When available, it is important to include the measurement of both biological parents of the child as a part of the assessment and to calculate the mid-parental height (see Chapter 3) to assess the child’s growth in the context of what would be expected for the family.
Investigate a growth velocity of less than 5 cm per year in children age 5 years to puberty; a growth velocity of less than 4 cm per year is clearly pathologic (see Chapter 3).
You cannot assess short stature or analyze growth velocity without examining the breasts and genitalia to determine the child’s pubertal stage (see Fig. 3–9).
Chief Characteristics of Thyroid Disorders in Children
Structure, function, signs, and symptoms
Evaluating a Child with Hyperthyroidism
Evaluating a Child with Hypothyroidism
Like children with hyperthyroidism, children with hypothyroidism rarely complain of symptoms (Box 16–1) perhaps because the changes develop so insidiously that neither child nor parent notices the difference. When symptoms go unrecognized for years, linear growth is profoundly impaired and may be the presenting feature.
Causes of Childhood Hypothyroidism
Case History 2
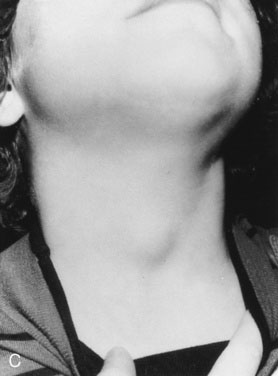
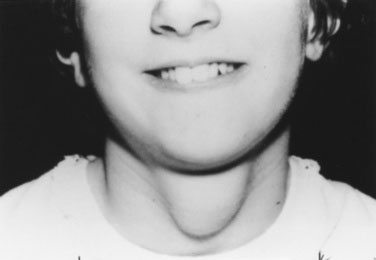
History. Shauna, age 15 years, says, “I was the tallest in my class in fifth grade, but I have not grown since then, and my periods haven’t started” (Fig. 16–5).
Your physical examination reveals all of the physical findings for hypothyroidism that are listed in Table 16–1. You particularly note the characteristic puffiness around Shauna’s upper face and eyes. In this case, because of profound hypothyroidism, there is also a more generalized swelling, including the neck.
TABLE 16–1 Causes of Precocious Puberty
| Type of Precocious Puberty | Underlying Cause |
|---|---|
| Central | Idiopathic Hypothalamic hamartoma Germinoma (pinealoma) Other cerebral tumors or malformations Severe hypothyroidism Secondary to cranial irradiation |
| Gonadal | Benign precocious thelarche (? central) Ovarian cysts, benign McCune-Albright syndrome (polyostotic fibrous dysplasia of bone, ovarian cysts, large irregular café-au-lait spots) Leydig cell hyperplasia (familial testotoxicosis) Gonadal tumors (male and female) Isolated premature menses (? central) |
| Adrenal | Benign premature adrenarche Congenital adrenal hyperplasia Adrenal tumors |
| Iatrogenic | Exogenous sources |
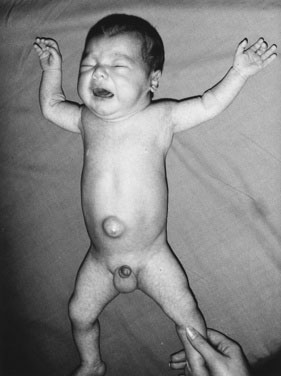
In a few infants, hypothyroidism is caused by a congenital enzyme defect in thyroid hormonogenesis. In such instances, a goiter is present. In many countries, congenital hypothyroidism is now detected in the presymptomatic stage, before any significant intellectual deficit occurs, through blood spot screening between the second and fifth days of life. If congenital hypothyroidism is left untreated, the clinical manifestations may not become fully apparent until around the third month of life.
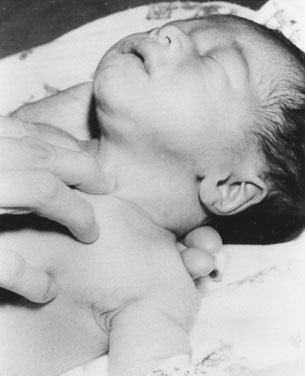
The infant with untreated congenital hypothyroidism has a low core body temperature, slow pulse rate, prolonged neonatal jaundice (because of poor hepatic conjugation of bilirubin), dry skin and hair, a large posterior fontanel (greater than 0.5 cm), poor head control, poor muscle tone, an enlarged tongue, a characteristically puffy face, and a hoarse cry (Fig. 16–6). The parents may report poor feeding and constipation. If acquired hypothyroidism develops after age 2 or 3 years, no permanent intellectual deficit is thought to occur.
Approach to the Physical Examination of the Child with a Thyroid Disorder
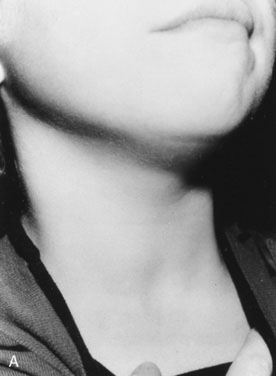
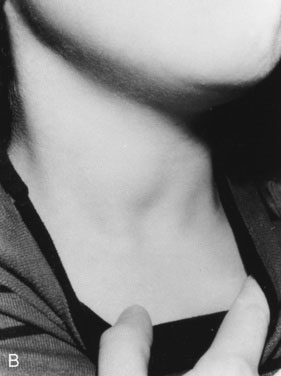
As with other pediatric examinations, always begin with the hands-off approach. Children are often ticklish, and touching the neck may elicit giggles and squirming, making it difficult to see the thyroid. Sit the child on a chair or examining table, with good light and in a relaxed atmosphere. If the child is old enough and cooperative, ask him or her to take a sip of water, first hold the water in the mouth without swallowing, and then swallow. Observe the area just above the sternal notch to see whether the small thyroid gland moves up and down during swallowing (Fig. 16–7). Next, ask the child to hyperextend the neck. This maneuver makes thyroid enlargement more obvious, and sometimes it is the only way to see the gland easily.
Examining newborns and young infants
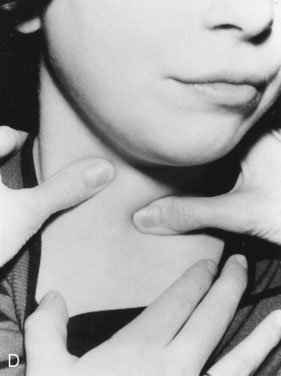
In a newborn or young infant, use a different technique to examine the thyroid. Place your hand under the child’s back, between the scapulae, and raise the baby’s shoulders, allowing the head to fall back gently until it rests on the examining table or a parent’s lap. If the thyroid is enlarged, this maneuver will expose it, allowing you to palpate with the second and third fingers of your other hand (Fig. 16–8).
Examining young children and adolescents
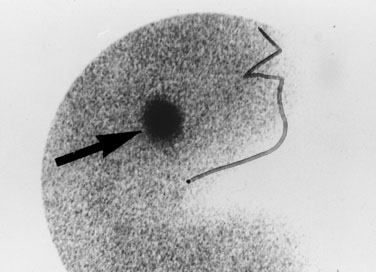
Most midline neck masses are thyroid glands or thyroid remnants. A central rounded midline mass between the thyroid and the chin is almost certain to be a thyroglossal duct cyst (Fig. 16–9), derived from a remnant of the thyroglossal duct, which runs from the foramen cecum of the tongue downward to the cricoid cartilage during fetal development. When the child sticks out the tongue, the mass moves upward. The child may present initially with an infected thyroglossal duct cyst. Sometimes, the gland fails entirely to migrate downward from the foramen cecum and manifests clinically as an oval or rounded midline mass at the base of the tongue (Fig. 16–10). This lingual thyroid usually represents all of the thyroid that the child has. Most lingual thyroids are treated with daily therapy using l-thyroxine, which suppresses pituitary thyrotropin (TSH) secretion, causing the lump to shrink markedly.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree