Chapter 333 Chronic Diarrhea
Pathophysiology
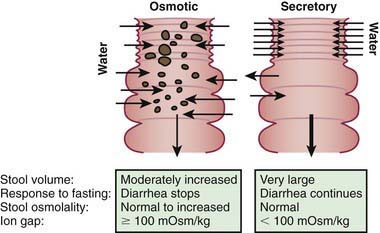
The mechanisms of diarrhea are generally divided into secretory and osmotic, but often diarrhea is the result of both mechanisms. Secretory diarrhea is usually associated with large volumes of watery stools and persists when oral food is withdrawn. Osmotic diarrhea is dependent on oral feeding, and stool volumes are usually not as massive as in secretory diarrhea (Fig. 333-1).
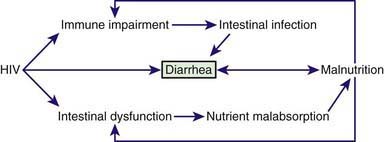
In many children, chronic diarrhea is induced by multiple mechanisms, intersecting each other and often producing a vicious cycle. A paradigm of chronic diarrhea generated by multiple mechanisms is provided by HIV infection, in which immune derangement, enteric infections, nutrient malabsorption, and intestinal damage, together with a direct enteropathogenic role of HIV, trigger and maintain chronic diarrhea (Fig. 333-2).
Etiology
A list of the main causes of chronic diarrhea is shown in Table 333-1.
Table 333-1 INFECTIOUS AND NONINFECTIOUS CAUSES OF CHRONIC DIARRHEA
INFECTIOUS ETIOLOGIES
DIARRHEA ASSOCIATED WITH EXOGENOUS SUBSTANCES
ABNORMAL DIGESTIVE PROCESSES:
NUTRIENT MALABSORPTION
IMMUNE AND INFLAMMATORY
STRUCTURAL DEFECTS
DEFECTS OF ELECTROLYTE AND METABOLITE TRANSPORT
MOTILITY DISORDERS
NEOPLASTIC DISEASES
CHRONIC NONSPECIFIC DIARRHEA
IPEX, immunodysregulation polyendocrinopathy enteropathy X-linked syndrome.
In small intestinal bacterial overgrowth, diarrhea may be the result of either a direct interaction between the microorganism and the enterocyte or the consequence of the deconjugation and dehydroxylation of bile salts and the hydroxylation of fatty acids due to an abnormal proliferation of bacteria in the proximal intestine (Chapter 330.4).
A reduction of intestinal absorptive surface is responsible for diarrhea in celiac disease, a permanent gluten intolerance that is sustained by a genetic basis affecting as many as 1/100 normal people, depending on geographic origin. Gliadin induces villous atrophy, leading to a reduction of functional absorptive surface area that is reversible upon implementation of a strict gluten-free diet (Chapter 330.2).
Chronic diarrhea may be the manifestation of maldigestion due to exocrine pancreatic disorders (Chapter 343). In most patients with cystic fibrosis, pancreatic insufficiency results in fat and protein malabsorption. In Shwachman-Diamond syndrome, exocrine pancreatic hypoplasia may be associated with neutropenia, bone changes, and intestinal protein loss. Specific isolated pancreatic enzyme defects result in fat and/or protein malabsorption. Familial pancreatitis, associated with a mutation in the trypsinogen gene, may be associated with pancreatic insufficiency and chronic diarrhea.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree