12 Child Abuse and Neglect
Physical Abuse
Clinical Presentation
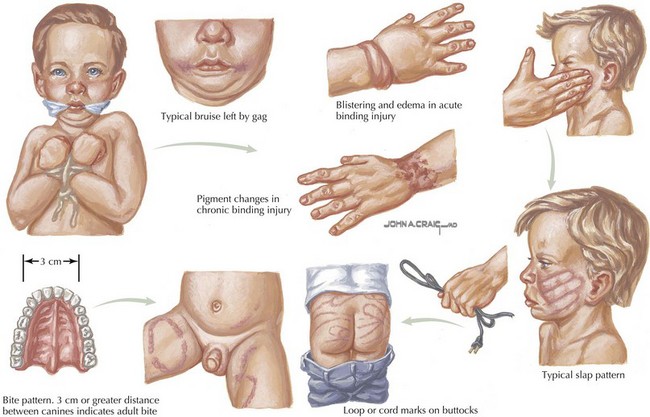
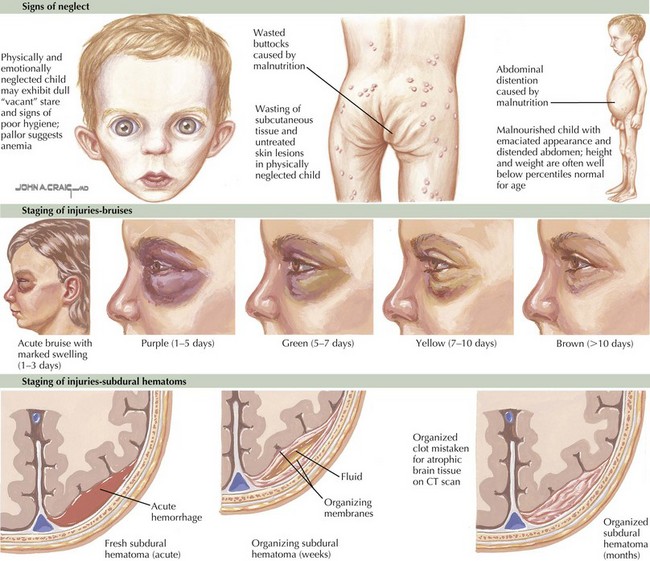
Remove all of the child’s clothing and examine the skin carefully for contusions, abrasions, burns, and lacerations in various stages of resolution. Any bruise on a child who is not yet cruising or walking is unusual. Certain skin lesions are typical for specific types of abuse; such as circular cigarette burns; human bite marks; J-shaped curvilinear or loop-shaped marks from a wire, cord, or belt; circumferential rope burns; “grid” marks from an electric heater; and symmetrical scald burns on the buttocks or extremities (Figure 12-1). Other dermatologic manifestations include cutaneous signs of malnutrition (decreased subcutaneous fat, increased creases), scalp hematomas, signs of trauma to the genital area, and signs of injuries at different stages of healing (Figure 12-2).
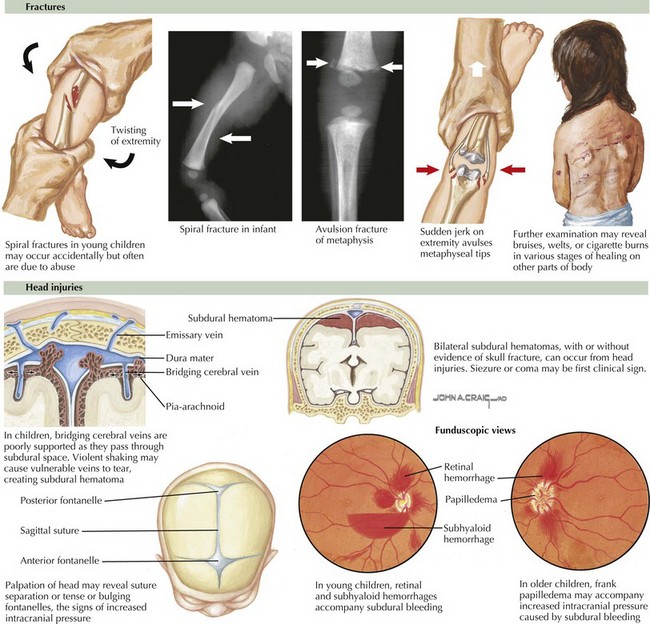
Fractures are suggested by refusal to bear weight or move an extremity, gross deformity, or soft tissue swelling and point tenderness over an extremity. However, most metaphyseal chip fractures are not associated with deformity (Figure 12-3). Neurologic manifestations may include retinal hemorrhages, unexplainable irritability, coma, or convulsions (see Figure 12-3). Finally, an acute abdomen, poisoning, or any traumatic injury that cannot be explained may in fact represent forms of child abuse.
Evaluation and Management
If the parents deny any knowledge of the cause of skin bruises, obtain a complete blood count with differential, platelet count, prothrombin time, partial thromboplastin time, and a bleeding time. The differential diagnosis and other possible laboratory studies are shown in Table 12-1.
Table 12-1 Differential Diagnosis and Abnormal Laboratory Studies to Support a Non-abuse Diagnosis
| Findings | Differential Diagnosis | Distinguishing Features and Tests |
|---|---|---|
| Bruising (extensive or deep) | Trauma | Physical examination |
| ITP | Decreased platelets | |
| Hemophilia | Increased PT, PTT | |
| Von Willebrand’s disease | Increased bleeding time | |
| Henoch-Schönlein purpura | Rash on lower extremities; rule out sepsis; normal platelet count | |
| Purpura fulminans | Clinical appearance (findings of sepsis); decreased platelet count | |
| Ehlers-Danlos syndrome | Joint hyperextensibility | |
| Dehydration | Renal or prerenal | Increased BUN, creatinine, urine specific gravity |
| Prerenal: BUN/creatinine >20:1 | ||
| Failure to thrive | Organic or nonorganic | History, physical examination; abnormal studies based on symptoms |
| Abdominal pain | Trauma | Hematuria; increased liver enzymes |
| Tumor | Increased amylase; abdominal ultrasonography; abnormal urinalysis | |
| Infection | Increased WBC, ESR; abdominal ultrasonography | |
| Fractures (multiple or in stages of healing) | Various trauma | |
| Osteogenesis imperfecta | Blue sclerae; radiography: decreased bone density | |
| Rickets | Increased calcium; decreased phosphorus, alkaline phosphatase | |
| Radiography: cupping at ends of long bones, widened metaphysic | ||
| Hypophosphatasia | Decreased calcium, alkaline phosphatase; increased phosphorus | |
| Leukemia | Abnormal peripheral smear, bone marrow, biopsy | |
| Previous osteomyelitis or septic arthritis | Increased WBC, ESR, CRP; positive culture | |
| Neurogenic sensory deficit | Detailed neurologic examination | |
| Metaphyseal or epiphyseal lesions | Trauma | Radiographs consistent with mechanism of injury |
| Scurvy | Radiographs: periosteal elevation; nutritional history | |
| Rickets | (See above) | |
| Menkes syndrome | Decreased copper, ceruloplasmin; hair analysis | |
| Syphilis | Abnormal serology | |
| Little League elbow | History of use | |
| Birth trauma | Neonatal history | |
| Subperiosteal ossification | Trauma | |
| Osteogenic malignancy | Radiographs; biopsy | |
| Syphilis | (See above) | |
| Infantile cortical hyperostosis | No metaphyseal changes | |
| Osteoid osteoma | Dramatic clinical response to aspirin | |
| Scurvy | (See above) | |
| CNS injury | Trauma | CT or MRI scan |
| Aneurysm | CT or MRI scan | |
| Tumor | MRI scan |
BUN, blood urea nitrogen; CNS, central nervous system; CT, computed tomography; ESR, erythrocyte sedimentation rate; MRI, magnetic resonance imaging; PT, prothrombin time; PTT, partial thromboplastin time; WBC, white blood cell.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree