Chapter 38 Cervical Dysplasia and Cancer
 Etiology and Epidemiology
Etiology and Epidemiology
Cervical cancer and its precursors have been associated with several epidemiologic variables (Box 38-1). These risk factors basically increase the likelihood of exposure to a high-risk HPV type.
The disease is relatively rare before 20 years of age, and the mean age is about 47 years.
 Cervical Topography
Cervical Topography
Throughout life, but particularly during adolescence and a woman’s first pregnancy, metaplastic squamous epithelium covers the columnar epithelium so that a new squamocolumnar junction is formed more proximally. This junction moves progressively closer to the external os and then up the endocervical canal. The transformation zone is the area of metaplastic squamous epithelium located between the original squamocolumnar junction and the new squamocolumnar junction (Figure 38-1).
 Classification of an Abnormal Papanicolaou Smear
Classification of an Abnormal Papanicolaou Smear
In 1988, a consensus meeting was convened by the Division of Cancer Control of the National Cancer Institute to review existing terminology and to recommend effective methods of cytologic reporting. As a result of this meeting, the Bethesda system was devised and requires (1) a statement regarding the adequacy of the specimen for diagnosis, (2) a diagnostic categorization (normal or other), and (3) a descriptive diagnosis. A revised Bethesda system was developed in 2001 and is shown in Box 38-2.
BOX 38-2 Bethesda Classification of Cytologic Abnormalities (2001, Abridged)
Epithelial Cell Abnormalities
Squamous Cell
CERVICAL INTRAEPITHELIAL NEOPLASIA
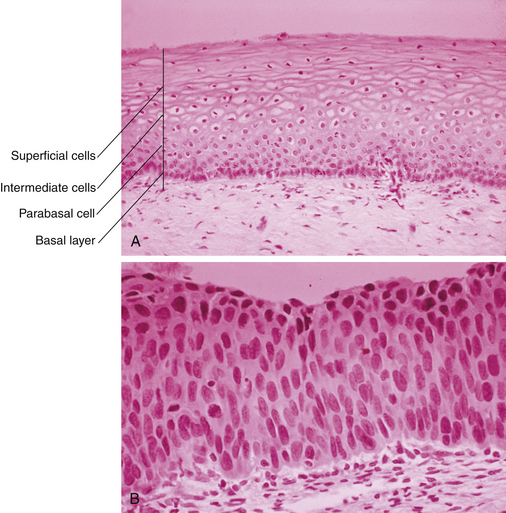
CIN represents a spectrum of disease, ranging from CIN I (mild dysplasia) to CIN III (severe dysplasia and carcinoma in situ). At least 35% of patients with CIN III develop invasive cancer within 10 years, whereas lower grades of CIN often spontaneously regress. With CIN, there is abnormal epithelial proliferation and maturation above the basement membrane. Involvement of the inner one third of the epithelium represents CIN I, involvement of the inner one half to two thirds represents CIN II, and full-thickness involvement represents CIN III (Figure 38-2). The disease is asymptomatic.
 Primary Prevention
Primary Prevention Screening of Asymptomatic Women
Screening of Asymptomatic Women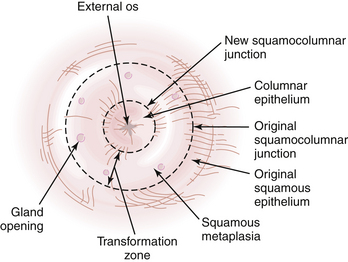
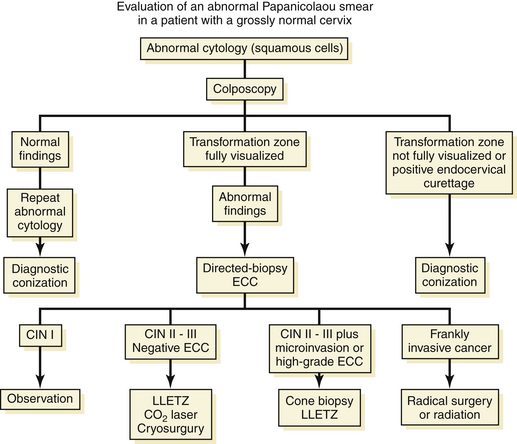
 Evaluation of a Patient with an Abnormal Papanicolaou Smear
Evaluation of a Patient with an Abnormal Papanicolaou Smear